5.1.Overview of Module 5
This module outlines the role and use of vitamin C in various cardiometabolic disorders, from obesity and metabolic syndrome/prediabetes, to the more severe conditions of type 2 diabetes and various cardiovascular diseases.
Following completion of this module the participant will be able to:
- Discuss the evidence-based role of vitamin C in cardiometabolic disease prevention and therapy to colleagues and patients (Communication, Scholarship, Professionalism)
- Describe the different ways vitamin C works in cardiometabolic conditions to colleagues and patients (Communication, Scholarship, Professionalism)
- Assess the potential usefulness of vitamin C administration to patients with cardiometabolic conditions in their healthcare practice (Management, Clinical expertise)
Length of activity: 15 min reading
RNZCGP Endorsed: 0.25 CME credits
CICM Accredited: 0.25 points
5.2. Vitamin C and cardiometabolic diseases
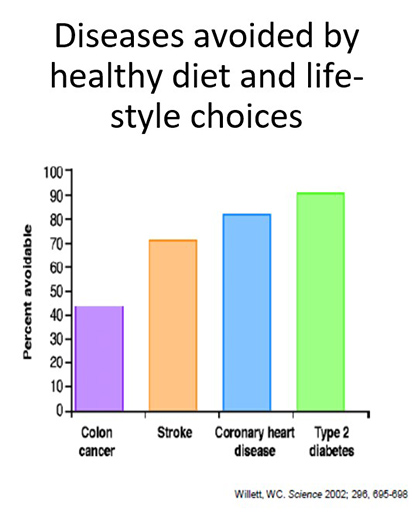
Research has indicated that cardiometabolic diseases such as type 2 diabetes, coronary heart disease and stroke can be almost fully prevented by healthy diet and lifestyle choices (see figure below). As you will learn below, high dietary intakes and plasma levels of vitamin C are associated with decreased risk and morbidity/mortality from cardiometabolic diseases such as obesity, metabolic syndrome, type 2 diabetes, hypertension and cardiovascular disease. Numerous meta-analyses have indicated that supplementation with vitamin C improves vitamin C status in these conditions and improves markers of glycaemic control, lipid profile, inflammation, endothelial function and blood pressure, particularly in people who have low vitamin C status and dysregulated markers at baseline.
5.3.Vitamin C and obesity
 The rising prevalence of obesity worldwide has been equated to a global pandemic. The World Health Organisation estimated that in 2016, 39% of the world's population were overweight and 13% were obese. Obesity is a major risk factor for other more severe cardiometabolic disorders, such as type-2 diabetes and cardiovascular disease, and is characterised by elevated inflammation and oxidative stress, both of which are typically associated with lower vitamin C status.
The rising prevalence of obesity worldwide has been equated to a global pandemic. The World Health Organisation estimated that in 2016, 39% of the world's population were overweight and 13% were obese. Obesity is a major risk factor for other more severe cardiometabolic disorders, such as type-2 diabetes and cardiovascular disease, and is characterised by elevated inflammation and oxidative stress, both of which are typically associated with lower vitamin C status.
5.3.1.Obesity observational studies
Large epidemiological studies (including the USA NHANES, the Canadian Health Measures Survey, the UK EPIC-Norfolk study, and the French SU.VI.MAX study baseline), have consistently indicated inverse correlations between body weight or BMI and vitamin C status (see further reading below for NZ-related data). Although low vitamin C status in people of higher body weight may be due to lower dietary intake of the vitamin, a volumetric dilution effect has also been proposed (see further reading below). This partly accounts for the typically lower vitamin C status in men relative to women.
Further reading:
- Vitamin C Status Correlates with Markers of Metabolic and Cognitive Health in 50-Year-Olds: Findings of the CHALICE Cohort Study. Pearson et al. Nutrients. 2017.
This epidemiological study showed that men had lower vitamin C status (see Figure 1), and this was also associated with elevated weight, BMI and waist circumference. - The lower vitamin C plasma concentrations in elderly men compared with elderly women can partly be attributed to a volumetric dilution effect due to differences in fat-free mass. Jungert and Neuhäuser-Berthold, Br J Nutr. 2015.
This epidemiological study investigated sex differences in vitamin C plasma concentrations and showed that higher fat-free mass was a major contributor to lower vitamin C status in men.
5.3.2.Obesity supplementation studies
The volumetric dilution premise is supported by a supplementation study by Block et al (1999), that indicated attenuated vitamin C status in overweight and obese people, despite comparable dietary intake to people of lower weight (see figure below). As such, the authors proposed that vitamin C recommendations should be based on a “dose per kg body weight” or in terms of “desirable plasma concentrations”. Our research has also indicated that the attenuated plasma response to low dose vitamin C supplementation in people with hypovitaminosis C was partly due to their higher body weight.
These studies suggest that people with higher body weight have higher requirements for vitamin C to reach comparable vitamin C status to those of normal body weight. This is an important consideration as the optimal kinetics of vitamin C-dependent enzymes is dependent on vitamin C concentrations. This may have important implications with regard to the setting of future RDA criteria. However, at present the optimal vitamin C intakes for people with obesity have not yet been determined. Estimates have been carried out based on the above Block (1999) data, in combination with the Levine (1996) pharmacokinetic data, and suggest that an additional 10 mg/day of vitamin C may be required for every additional 10 kg of body weight (within the range of 60 to 90 kg; see figures below). Obesity is characterised by elevated inflammation and oxidative stress, which may increase vitamin C requirements further.
Further reading
- Body weight and prior depletion affect plasma ascorbate levels attained on identical vitamin C intake: a controlled-diet study. Block et al. J Am Coll Nutr, 1999.
This is one of the few studies that has assessed the response to vitamin C supplementation based on body weight and showed lower response by those with higher body weight. - Marginal ascorbate status (hypovitaminosis C) results in an attenuated response to vitamin C supplementation. Carr et al. Nutrients, 2016.
This study showed that the attenuated plasma response to low dose vitamin C supplementation in people with hypovitaminosis C (see Figure 1) was partly due to their higher body weight. - Estimation of Vitamin C Intake Requirements Based on Body Weight: Implications for Obesity. Carr et al. Nutrients, 2022.
This study reanalysed the Block (1999) data, in combination with the Levine (1996) pharmacokinetic data, to estimate vitamin C requirements for higher body weight.
5.4.Vitamin C and metabolic syndrome
Metabolic syndrome (MetS; also referred to as pre-diabetes) is a chronic condition comprising a constellation of cardiometabolic risk factors characterised by abdominal obesity, insulin resistance, hypertension and dyslipidemia. MetS has become a major public health challenge worldwide, estimated to affect 20-25% of the world's adult population, increasing to 30–40% by age 65. It is a risk factor for more severe chronic diseases such as type 2 diabetes mellitus (5-fold greater risk) and various cardiovascular diseases (CVDs). Obesity is a major risk factor for MetS, with the risk of developing MetS increasing strikingly above a BMI of 25. MetS is also characterised by chronic low-grade inflammation which is believed to contribute to insulin resistance and vascular dysfunction. Thus, targeting inflammatory and/or oxidative processes at the MetS/prediabetes stage may help attenuate progression to the more severe cardiometabolic diseases of type 2 diabetes or CVD.
5.4.1.MetS observational studies
Epidemiological research and subsequent meta-analysis have highlighted that people with MetS tend to have lower vitamin C status relative to healthy controls. A higher baseline vitamin C status was also associated with a lower prevalence of MetS (OR=0.53; 95% CI 0.35, 0.80) in 5,220 adults participating in the SU.VI.MAX primary prevention trial. Meta-analysis of 11 observational studies indicated an inverses association between circulating vitamin C and MetS risk (RR = 0.60, 95% CI: 0.49, 0.74).
Further reading:
- Vitamin C and metabolic syndrome: A meta-analysis of observational studies. Guo et al. Front Nutr, 2021.
This meta-analysis (of 23 observational studies) indicated that dietary and, in particular, circulating vitamin C levels were inversely associated with MetS.
5.4.2.MetS supplementation studies
Meta-analyses have indicated that vitamin C supplementation can improve markers of metabolic health (glycaemic control and lipid profiles), particularly in people with low vitamin C status or dysregulated metabolic markers at baseline. Meta-analysis has also indicated that vitamin C intervention can decrease levels of inflammatory markers, such as CRP, in different populations. Two RCTs specifically investigating vitamin C supplementation (500 mg/day) of people with MetS have indicated decreased BMI and improved lipid profiles (decreased TG and LDL-C) compared with the placebo group (see further reading below). More high-quality studies in people with MetS are required.
Further reading:
- Vitamin C: A review on its role in the management of metabolic syndrome. Wong et al. Int J Med Sci, 2020.
A narrative review on the role of vitamin C in MetS studies, including intake, status and intervention studies
5.5.Vitamin C and type 2 diabetes
Type-2 diabetes is a complex disorder characterised by chronic metabolic dysregulation and potentially life-threatening microvascular and macrovascular complications (such as nephropathy, retinopathy, neuropathy and CVD). The prevalence of type 2 diabetes continues to increase globally, with worldwide cases of diabetes comprising almost half a billion people in 2019. Risk factors for type 2 diabetes include obesity and metabolic syndrome.
5.5.1.Diabetes observational studies
Large epidemiological studies (e.g. EPIC-Norfolk comprising approximately 20,000 British adults, and EPIC-InterAct, including eight European countries) have established inverse associations between vitamin C intake or plasma concentrations and risk of developing type-2 diabetes (see further reading below). Despite generally higher dietary and supplemental vitamin C intakes following diagnosis, people with diabetes tend to have lower vitamin C status than those without diabetes, indicating that other factors, such as the elevated inflammation and oxidative stress observed in this condition, could be increasing requirements for the vitamin.
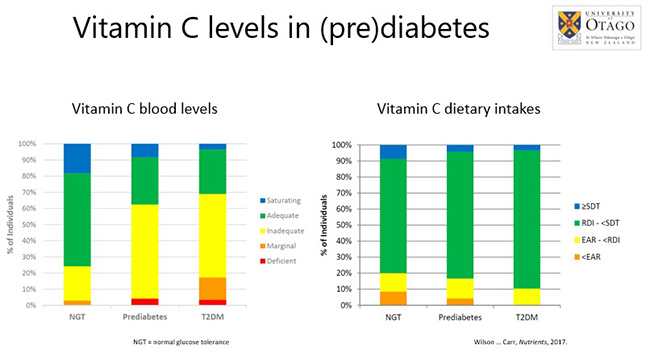
Our research has indicated that people with prediabetes or T2DM exhibited lower vitamin C status and a higher prevalence of deficiency and insufficiency than healthy controls with normal glucose control. This was despite comparable dietary intakes of the vitamin to healthy controls (see Figure below). This suggests a higher utilisation of the vitamin in diabetes, and is observed even at the pre-diabetes stage, possibly due to inflammatory and oxidative stress processes occurring early in the disease process.
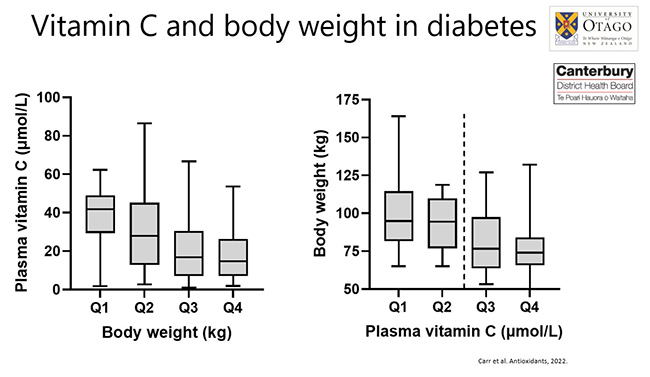
Furthermore, our recent research has indicated lower vitamin C status in people with type 2 diabetes relative to type 1 diabetes, and also inverse associations between body weight and vitamin C status in people with diabetes, suggesting a volumetric dilution contribution. People with hypovitaminosis C (≤23 µmol/L; dashed line in figure below) had significantly higher body weight. Weight accounted for one third of the difference in vitamin C status between people with type 1 and type 2 diabetes. Of note, subgroup analyses indicated that NZ Māori and Pasifika participants (as a group) had lower vitamin C status. Body weight/BMI were higher in the NZ Māori/Pasifika subgroup, which likely contributed to their lower vitamin C status. These findings suggest that people with both diabetes and a high body weight may have greater than average vitamin C requirements, and supplementation may be required to restore adequate vitamin C status. The doses required remain to be established.
Further reading:
- Plasma vitamin C level, fruit and vegetable consumption, and the risk of new-onset type 2 diabetes mellitus: the European prospective investigation of cancer--Norfolk prospective study. Harding et al. Arch Intern Med. 2008.
This epidemiological study showed that plasma vitamin C status was a better predictor for diabetes risk than dietary intake. - Inadequate Vitamin C Status in Prediabetes and Type 2 Diabetes Mellitus: Associations with Glycaemic Control, Obesity, and Smoking. Wilson et al. Nutrients, 2017.
This observational study showed that vitamin C insufficiency was apparent even at the prediabetes stage, and was independent of dietary intake, but was associated with BMI. - Vitamin C Status in People with Types 1 and 2 Diabetes Mellitus and Varying Degrees of Renal Dysfunction: Relationship to Body Weight. Carr et al. Antioxidants, 2022.
This observational study showed lower vitamin C status in people with T2DM relative to T1DM, and higher body weight was a significant predictor of low vitamin C status.
5.5.2. Diabetes supplementation studies
Numerous vitamin C intervention studies have been carried in people with type 2 diabetes. Meta-analyses of these studies have indicated that vitamin C supplementation (typically doses of 500 – 1000 mg/d) improved glycaemic control, lipid profiles and blood pressure in people with type 2 diabetes. Effects on lipid profile were dependent on dose and duration of vitamin C administration. The effect sizes were also related to baseline BMI. All of these markers are risk factors for the more severe complications of diabetes. Therefore, attenuation of these, as well as markers of inflammation, may attenuate progression of diabetes to its more severe complications.
To date, only a few preliminary studies have assessed the effect of vitamin C supplementation (500 - 1000 mg/d) on inflammatory biomarkers in obese and/or diabetic adults. Two showed decreased CRP, TNF-α and IL-6, while the third showed no effect of intervention, although this was the lower dose and a smaller cohort (n=12 treated). Two of the studies did not assess the vitamin C status of the participants at baseline, which as you learnt in Module 1 can affect the outcome of vitamin intervention studies.
Diabetic foot ulcers are a major complication of severe diabetes and precedes most diabetes-related lower-leg amputations. Research in Australia has indicated a very high prevalence of vitamin C deficiency in people with diabetic foot ulcers (50%) and an RCT supplementing people with foot ulcers and deficient vitamin C status showed dramatic improvement in wound healing and zero amputations. Preclinical research has indicated that vitamin C can aid wound healing through multiple mechanisms. These include stimulating the synthesis and maturation of collagen, aiding leukocyte function and attenuating infections.
Further reading:
- Effects of vitamin C supplementation on glycemic control and cardiovascular risk factors in people with type 2 diabetes: A GRADE-assessed systematic review and meta-analysis of randomized controlled trials. Mason et al. Diabetes Care. 2021.
This meta-analysis of 28 studies indicated beneficial effects of vitamin C supplementation on HbA1c and systolic and diastolic blood pressure. - Does vitamin C supplementation exert profitable effects on serum lipid profile in patients with type 2 diabetes? A systematic review and dose-response meta-analysis. Namkhah et al. Pharmacol Res. 2021.
This meta-analysis of 15 studies indicated beneficial effects of vitamin C supplementation on the profile of selected lipids and highlighted the importance of dose and duration of administration.
5.6.Vitamin C and hypertension
Hypertension is a major comorbidity of obesity and diabetes and is a significant risk factor for cardiovascular disease incidence and mortality. The Global Burden of Disease research has highlighted hypertension as one of the leading global risk factors for mortality.
5.6.1.Hypertension observational studies
The EPIC-Norfolk study (>20,000 participants) has revealed inverse associations between vitamin C status and blood pressure, with the likelihood of having hypertension being 22% lower (odds ratio: 0.78 [95% CI: 0.71 to 0.86]) for those who were in the top quartile of plasma vitamin C levels compared with the bottom quartile, after adjusting for multiple confounders. Our research has shown that patients with diabetes who had hypertension had median vitamin C levels approx. half that of normotensive patients with diabetes (17 vs 30 µmol/L). Meta-analysis of 18 observational studies has indicated an inverse association between vitamin C status and both systolic and diastolic blood pressure, with people with hypertension having a lower vitamin C status (by 15 µmol/L) than normotensive people (see further reading below).
Further reading:
- Association between Serum Vitamin C and the Blood Pressure: A Systematic Review and Meta-Analysis of Observational Studies. Ran et al. Cardiovasc Ther, 2020.
This meta-analysis of 15 studies showed lower vitamin C status in people with hypertension, and an inverse association between vitamin C levels and systolic and diastolic blood pressure.
5.6.2.Hypertension supplementation studies
Numerous trials have investigated vitamin C intervention for hypertension. Meta-analysis of 29 RCTs investigating vitamin C supplementation (median dose 500 mg/d) on blood pressure indicated a significant reduction of blood pressure (particularly systolic blood pressure), with the largest effects being seen in patients with hypertension (see further reading below).
Further reading:
- Effects of vitamin C supplementation on blood pressure: a meta-analysis of randomized controlled trials. Juraschek et al. Am J Clin Nutr, 2012.
This meta-analysis of 29 trials showed decreased diastolic and systolic blood pressure in people supplemented with vitamin C, with the largest effects being seen in those with hypertension.
5.7.Vitamin C and cardiovascular disease
Cardiovascular diseases (CVDs), principally ischemic heart disease and stroke, are the leading cause of global mortality and disease burden. In 2019, the Global Burden of Disease data indicated that cases had increased to over half a billion people with nearly 20 million deaths attributed to CVD.
5.7.1.CVD observational studies
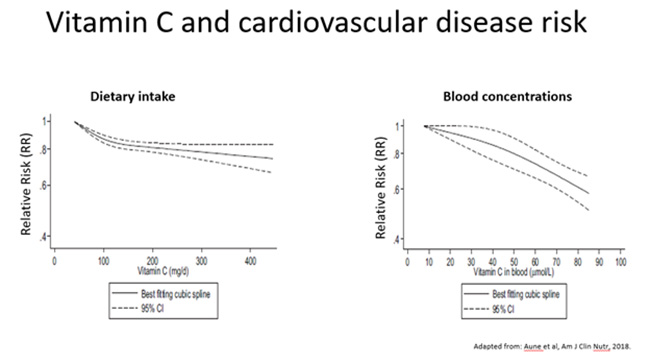
Multiple analyses of the EPIC-Norfolk study data have revealed inverse associations between vitamin C status and risk of stroke, coronary artery disease, and heart failure, and mortality from cardiovascular disease and ischaemic heart disease. Meta-analyses have supported that higher vitamin C intake and circulating concentrations are associated with a lower risk of coronary heart disease, stroke and cardiovascular disease (see figure below), and a lower risk of cardiovascular disease mortality (see further reading below). Aune et al. (2019) reported that the relative risk per 100 mg/day increment of dietary vitamin C intake was 0.88 (95% CI: 0.79, 0.98, n = 11) for coronary heart disease, 0.92 (95% CI: 0.87, 0.98, n = 12) for stroke and 0.89 (95% CI: 0.85, 0.94, n = 10) for cardiovascular disease. The corresponding relative risks per 50 μmol/L increase in blood concentrations of vitamin C were 0.74 (95% CI: 0.65, 0.83, n = 4), 0.70 (95% CI: 0.61, 0.81, n = 4), and 0.76 (95% CI: 0.65, 0.87, n = 6), respectively. Similarly, a dose-response meta-analysis indicated that circulating vitamin C was more strongly associated with risk of cardiovascular disease mortality than dietary intakes: 0·60 (95 % CI 0·42, 0·78; n = 6) vs 0·79 (95 % CI 0·68, 0·89; n = 10).
Further reading:
- Dietary and circulating vitamin C, vitamin E, β-carotene and risk of total cardiovascular mortality: a systematic review and dose-response meta-analysis of prospective observational studies. Jayedi et al. Public Health Nutr, 2019.
This meta-analysis demonstrates that higher vitamin C intake and higher circulating concentrations are associated with a lower risk of CVD mortality.
5.7.2.CVD supplementation studies
Few trials have investigated supplementation with oral vitamin C as a monotherapy for cardiovascular disease. An intervention trial carried out in people with hypercholesterolemia supplemented with 500 mg/d vitamin C indicated a trend towards decreased atherosclerotic progression. Notably, the effects were larger in participants with low baseline vitamin C.
As mentioned in earlier sections, meta-analyses of RCTs have indicated that vitamin C supplementation can improve cardiovascular disease risk factor markers (e.g. C-reactive protein, lipid profiles, endothelial function), particularly in subgroups with elevated CVD risk, older people, those with obesity, and lower baseline vitamin C status (see further reading below). However, meta-analysis of eight RCTs using vitamin C as a single nutrient for at least three months in healthy adults or those of moderate or high risk of cardiovascular disease indicated no evidence to suggest that vitamin C supplementation reduced the risk of cardiovascular disease risk factors or cardiovascular disease itself (the latter comprised one study only: the Physicians Health Study II).
In contrast, recent meta-analysis has indicated that vitamin C supplementation may help in heart failure as observed by improved left ventricular ejection fraction (see further reading below). In six cardiac trials with 246 patients, vitamin C increased LVEF on average by 12.0% (95% CI 8.1–15.9%). In six non-cardiac trials including 177 participants, vitamin C increased LVEF on average by 5.3% (95% CI 2.0–8.5%). There was a strong negative association between the size of the vitamin C effect and the baseline LVEF.
Further reading
- Limited evidence for a beneficial effect of vitamin C supplementation on biomarkers of cardiovascular diseases: an umbrella review of systematic reviews and meta-analyses. Ashor et al. Nutr Res, 2019.
This umbrella review highlights evidence that certain population subgroups (e.g. older people, obese people, those with lower baseline vitamin C status, and those at higher CVD risk) may be more responsive to vitamin C supplementation. - Vitamin C May Improve Left Ventricular Ejection Fraction: A Meta-Analysis. Hemilä et al. Front Cardiovasc Med, 2022.
This meta-analysis of 12 trials indicated that vitamin C increased LVEF in both cardiac and non-cardiac patients.
5.7.3.Use of vitamin C in post-cardiac surgery
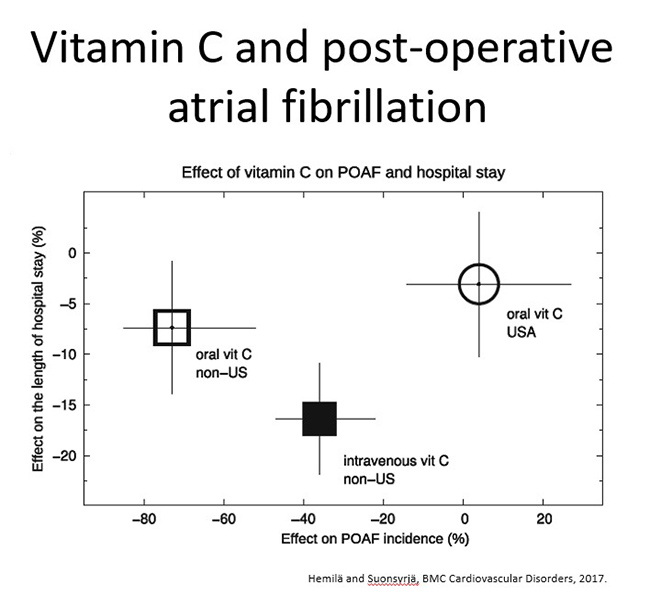
Post-operative atrial fibrillation (POAF), a cardiac arrhythmia, is a common complication after cardiac surgery. Both oral and intravenous vitamin C have been used in studies to assess its effects on POAF due to its association with oxidative stress. Of note, studies carried outside the US appear to have the best outcomes with regard to both incidence of POAF and length of hospital stay post-cardiac surgery (see figure and further reading below).
Further reading
- Vitamin C for preventing atrial fibrillation in high risk patients: a systematic review and meta-analysis. Hemilä and Suonsyrjä. BMC Cardiovasc Disord, 2017.
This meta-analysis of 15 trials in high risk patients indicated that both oral and IV vitamin C may prevent post-operative atrial fibrillation in some countries outside of the USA, and it may also shorten the duration of hospital stay and ICU stay of cardiac surgery patients.
5.7.4.Vitamin C mechanisms of action in CVD
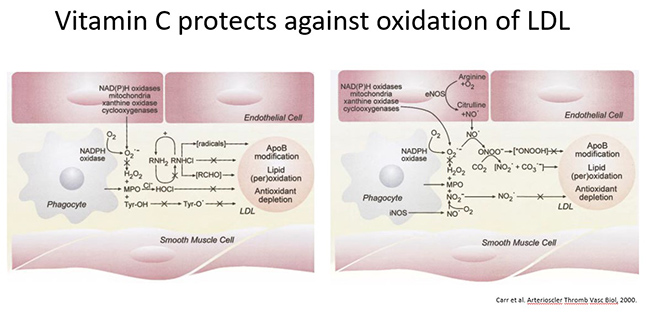
Numerous anti-atherogenic mechanisms have been proposed for vitamin C, which primarily focus on its anti-inflammatory and antioxidant properties. These include: attenuating leukocyte adhesion to the vasculature and preventing LDL oxidation by leukocyte-derived oxidants within the intima (see figure below for reaction pathways).
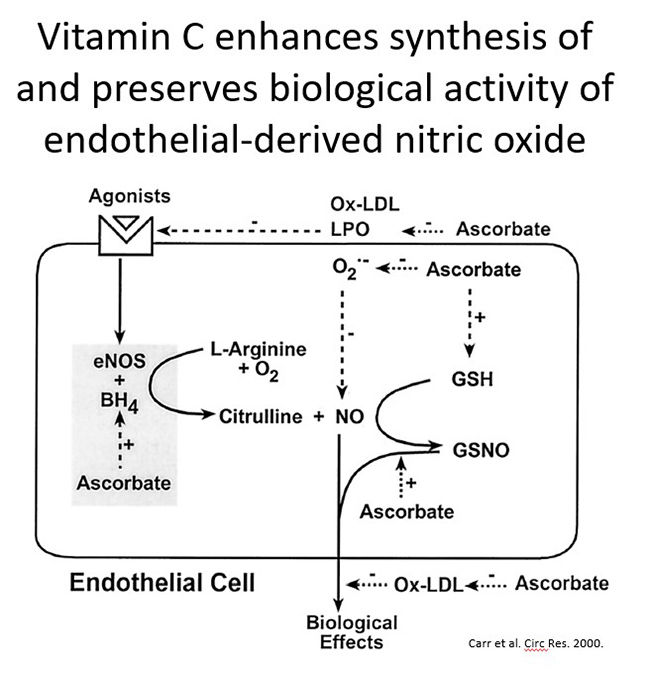
Vitamin C also supports endothelial-derived nitric oxide (NO) synthesis and activity (see figure below). Tetrahydrobiopterin is a cofactor for hydroxylating enzymes such as nitric oxide synthase. Vitamin C is able to regenerate tetrahydrobiotperin from its oxidised state, thus potentially aiding NO synthase activity. The effects of oral and intravenous vitamin C on endothelial function have been assessed via measuring flow-mediated dilation.
5.8. Summary of Module 5
- Epidemiological studies indicate inverse associations between vitamin C status and body weight or BMI. This is likely partly due to a volumetric dilution effect and may also account for the typically lower vitamin C status of men relative to women.
- Administration of vitamin C to people of higher body weight results in lower circulating concentrations relative to people of lower body weight. Thus, people with higher body weight will likely need higher intakes than those currently recommended.
- People with metabolic syndrome, encompassing both higher body weight and metabolic dysregulation, tend to have lower vitamin C status. Limited vitamin C trials have indicated potential improvement in BMI and lipid profiles. Further trials are required.
- Epidemiological studies indicate that people with higher vitamin C intake or plasma status have lower risk of developing type-2 diabetes. People with type-2 diabetes tend to have lower vitamin C levels than healthy controls, despite comparable dietary intakes of the vitamin. This appears to be partly due to higher body weight.
- Meta-analyses of vitamin C supplementation of people with type-2 diabetes have indicated improved glycaemic control, lipid profiles, blood pressure, and possibly also inflammatory biomarkers. The efficacy was related to baseline parameters e.g. dyslipidaemia, body weight.
- Similar findings have been reported for people with hypertension: an inverse association of vitamin C status with blood pressure and lower vitamin C levels in people with hypertension relative to normotensive people. Meta-analyses indicate a significant reduction in blood pressure following vitamin C supplementation, particularly in those with hypertension.
- Epidemiological studies indicate a decreased risk of cardiovascular disease (CVD) with higher vitamin C intake and plasma status. Meta-analyses show vitamin C supplementation decreases CVD risk factors and may also help in heart failure as observed by improved left ventricular ejection fraction, as well as potentially improve post-operative atrial fibrillation.
- Vitamin C has a number of potential mechanisms of action in the cardiovascular system that primarily focus on its antioxidant and anti-inflammatory properties. These include attenuating leukocyte adhesion to the vasculature, preventing LDL oxidation, and supporting endothelial derived nitric oxide (NO) synthesis and activity.
5.8.1. Optional activity: overview audiovisual
Timing: approximately 55min
Watch this presentation:
5.9.Activity: Self-reflection and feedback
Once you have completed all the Modules of interest to you, please complete the self-reflection and feedback form online or email to anitra.carr@otago.ac.nz. For members of the RNZCGP, please include your MCNZ number and the modules completed so that your CPD credits can be uploaded to the RNZCGP website. A certificate of completion can be emailed to you if required.
© Anitra Carr, 2022. You may not copy, modify, distribute, display, transmit, perform, publish or sell any of the copyrightable material on this website. You may hyperlink to this website but must include the following statement: "This link leads to the website 'Oral and intravenous vitamin C use in health care' provided by the Nutrition in Medicine Research Group at University of Otago, Christchurch."
