Professor Stephen Robertson, Group Leader
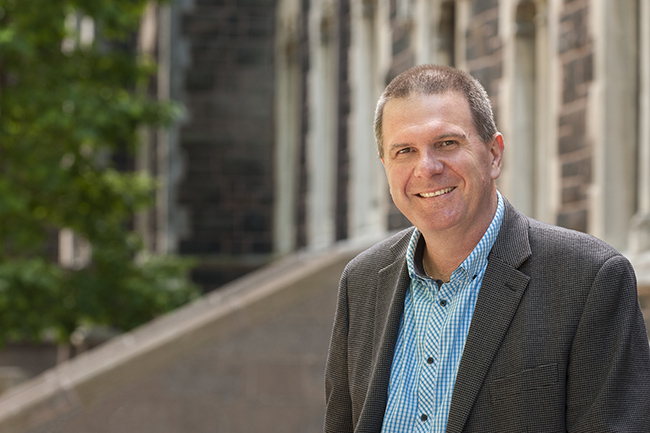
Professor Stephen Robertson.
Email stephen.robertson@otago.ac.nz
Stephen Robertson is the Child Health Research Foundation Professor of Paediatric Genetics at the University of Otago in Dunedin. He was educated at the University of Otago, graduating in Medicine in 1990. He specialised in Paediatrics and Genetics after training at various hospitals in greater Auckland and at the Victorian Clinical Genetics Service in Melbourne from 1997–1999. From 1995–1996, he was Chief Resident of Starship Children's Hospital in Auckland.
From 1999–2002, Stephen was Nuffield Medical Fellow at St Catherine's College, Oxford University, studying the genetic determinants of congenital malformations in children. This work was conducted in the laboratory of Professor Andrew Wilkie at the Weatherall Institute of Molecular Medicine. It culminated in the publication of two papers in Nature Genetics in 2003 and 2004 outlining the role of a new family of genes, the filamins, in the generation of these conditions. He remains an active clinical geneticist attached to Genetic Health Services New Zealand, as well as continuing his research into congenital malformations.
View Professor Stephen Robertson's staff profile
The Curekids Chair in Child Health Research
![]()

Curekids Fundraiser.
The Child Health Research Foundation (subsequently re-branded as Curekids) launched an initiative in 2002 to establish a chair at the University of Otago that was dedicated to aspects of child health research. A large number of corporate organisations and private individuals contributed to the establishment of the position. Most notably, four men from Queenstown – Graham Smolenksi, Jeff Turner, Wayne Cafe, and Fraser Skinner – initiated an international ski endurance event – The 50k of Coronet – over five successive years from 2000–2004 to contribute over $1 million to the fund. Professor Robertson was appointed as the Inaugural Curekids Professor in late 2002 and established the Clinical Genetics Group. In 2006, in collaboration with the Government's Partnerships in Excellence Programme and the University's Leading Thinkers Programme, the Curekids Chair in Child Health Research was established in perpetuity.
Read more about the Curekids Chair in Child Health Research at the Curekids website
Current staff
Zandra Jenkins
Research Fellow
Email zandra.jenkins@otago.ac.nz
 I began my research studying the molecular genetics of wool at the AgResearch Molecular Biology Unit, University of Otago, completing my doctorate in 1998. I went on to carry out postdoctoral research at the Department of Cell and Molecular Biology, Uppsala University Sweden (1998–2000) studying protein translation. I continued this research at the Childrens Hospital Oakland Research Institute, USA (2000–2002), in addition to studying the regulation of iron homeostasis in patients with sickle cell anaemia and β-thalassemia. Returning to New Zealand in 2003, I joined the Clinical Genetics Group as a Research Fellow.
I began my research studying the molecular genetics of wool at the AgResearch Molecular Biology Unit, University of Otago, completing my doctorate in 1998. I went on to carry out postdoctoral research at the Department of Cell and Molecular Biology, Uppsala University Sweden (1998–2000) studying protein translation. I continued this research at the Childrens Hospital Oakland Research Institute, USA (2000–2002), in addition to studying the regulation of iron homeostasis in patients with sickle cell anaemia and β-thalassemia. Returning to New Zealand in 2003, I joined the Clinical Genetics Group as a Research Fellow.
Emma Wade
Postdoctoral Fellow
Email emma.wade@otago.ac.nz
 Emma completed her undergraduate degree in genetics at the University of York in 2010. She spent the next two years working in the clinical genetics group at Manchester University as a research assistant, studying the genetic cause of glaucoma.
Emma completed her undergraduate degree in genetics at the University of York in 2010. She spent the next two years working in the clinical genetics group at Manchester University as a research assistant, studying the genetic cause of glaucoma.
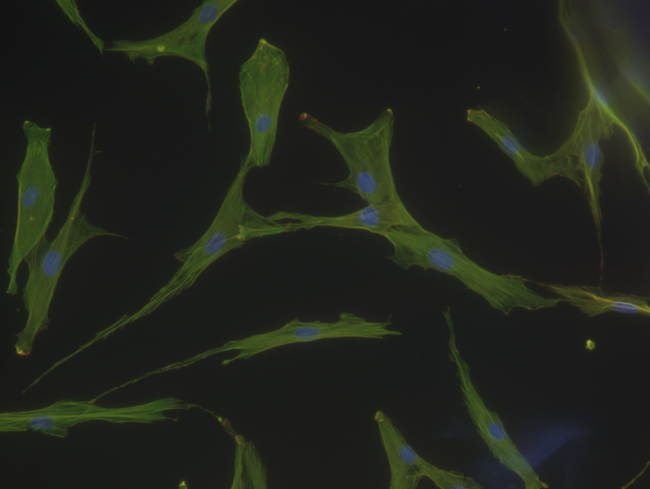
In 2013 she moved to the University of Otago to complete her PhD with Prof. Stephen Robertson in the Department of Women's and Children's Health. Her PhD research focused on the genetic cause of rare, childhood bone diseases and how these genetic mechanisms contribute to how the skeleton senses force. Her PhD uncovered mutations in two genes which lead to an exciting hypothesis and ultimately a Marsden funded project for the Clinical Genetics group.
She is now employed as a postdoctoral fellow pursuing a project which has grown out of her PhD: trying to untangle the signalling pathways which maintain skeletal homeostasis.
Ben Halliday
Postdoctoral Fellow
Email benjamin.halliday@otago.ac.nz
 I completed my BSc(Hons) in 2016, exploring the genetic drivers of childhood kidney cancers. Through this project I developed a passion for bioinformatics, particularly in the application of genome sequencing techniques to explore rare disease genetics.
I completed my BSc(Hons) in 2016, exploring the genetic drivers of childhood kidney cancers. Through this project I developed a passion for bioinformatics, particularly in the application of genome sequencing techniques to explore rare disease genetics.
In 2017, I began my PhD in the Laboratory for Genomic Medicine. My doctoral research focused on the genomic investigation of patients with brain malformations, providing diagnostic answers for patients and their families, as well as improving understanding of the genetic pathways critical for brain development.
I am now a Postdoctoral Fellow in the Laboratory for Genomic Medicine, and contribute to several ongoing projects in the lab. My main project involves assessing the appropriateness of first-tier genomic diagnostic tools in New Zealand, and investigating why these tools have reduce performance in Māori and other Pacific Peoples.
Elizabeth Goodin
Assistant Research FellowEmail liz.goodin@otago.ac.nz
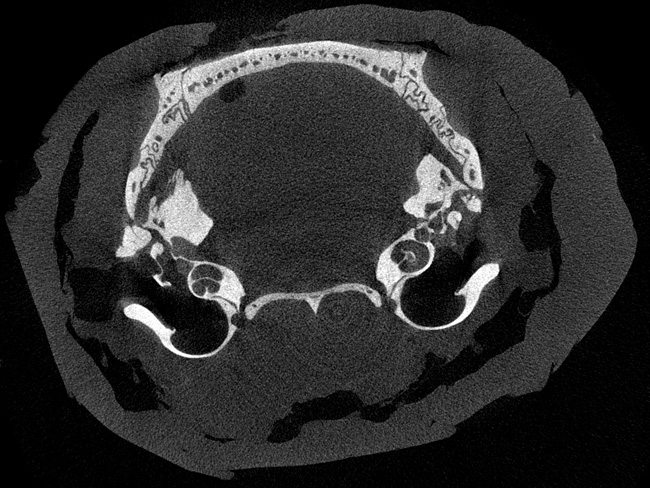
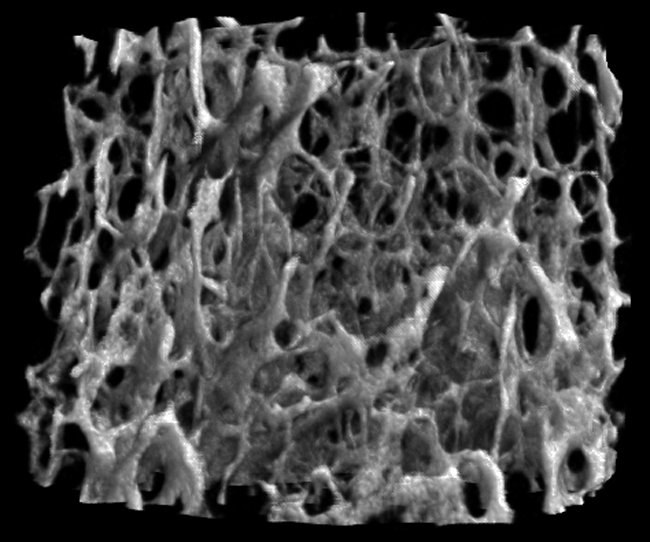
 I joined the Clinical Genetics Group as a Research Technician in 2019, working mainly with mouse models which help us learn more about skeletal development. One interesting technique I use is Micro CT, which is 3D x-ray scanning of small (micro) structures, in our case mouse bones. These scans allow us to compare bones between groups of mice with or without a particular genetic change and investigate how certain genes might be important in bone structure.
I joined the Clinical Genetics Group as a Research Technician in 2019, working mainly with mouse models which help us learn more about skeletal development. One interesting technique I use is Micro CT, which is 3D x-ray scanning of small (micro) structures, in our case mouse bones. These scans allow us to compare bones between groups of mice with or without a particular genetic change and investigate how certain genes might be important in bone structure.
Previously, from 2017–2019, I carried out work in our lab on behalf of the world famous Dunedin Longitudinal Study, which studies human health, development and behaviour. In this role, I processed and catalogued past and present study member samples, including DNA. Prior to that, I completed a master's degree with the Robertson group, taking a close look at the gene MET, which is important in a bone disease called Osteofibrous Dysplasia (OFD). Among other techniques, I used specially designed antisense oligonucleotides to target certain RNA sites in cells, in search of what might regulate the differential processing of this gene to cause disease.
Padmini Parthasarathy
Assistant Research Fellow
Email mini.parthasarathy@otago.ac.nz
 I was introduced to clinical genomics while I worked for a diagnostic company in India after completing my postgraduation in Biotechnology. I then moved to New Zealand to pursue my Research Master's with Prof Tony Merriman at the University of Otago, where I studied the association of genetic variants with blood urate levels in the New Zealand Māori and Pacific population. In May 2018, I joined the Clinical Genetics Group as a clinical bioinformatician, primarily involved in wrangling, processing and analysing whole genome sequences to aid in the genetic diagnosis of patients as well as the discovery of new genes associated with developmental disorders.
I was introduced to clinical genomics while I worked for a diagnostic company in India after completing my postgraduation in Biotechnology. I then moved to New Zealand to pursue my Research Master's with Prof Tony Merriman at the University of Otago, where I studied the association of genetic variants with blood urate levels in the New Zealand Māori and Pacific population. In May 2018, I joined the Clinical Genetics Group as a clinical bioinformatician, primarily involved in wrangling, processing and analysing whole genome sequences to aid in the genetic diagnosis of patients as well as the discovery of new genes associated with developmental disorders.
Tim Morgan
Research Technician
Email tim.morgan@otago.ac.nz
 I completed my MSc in Biochemistry in Professor Julian Eaton-Rye's lab in 2000, working on photosysthesis research. From there, I started working in Professor Robin Old's lab on bipolar disorder. Then I moved to Professor Stephen Robertson's new lab in 2003, working mainly with Filamin A, Filamin B and WTX.
I completed my MSc in Biochemistry in Professor Julian Eaton-Rye's lab in 2000, working on photosysthesis research. From there, I started working in Professor Robin Old's lab on bipolar disorder. Then I moved to Professor Stephen Robertson's new lab in 2003, working mainly with Filamin A, Filamin B and WTX.
Professor Mac Gardner
Adjunct Professor
Email macgardner@gmail.com
 Professor Gardner is a semi-retired medical geneticist. He is an Otago graduate, who was previously a member of the Paediatrics Department (1977–1993), before moving to the Genetic Service based at the Royal Children's Hospital in Melbourne (1993–2007). He has broad clincal interests, with a particular focus on inherited cerebellar ataxias and chromosomal disorders. He co-authors the textbook 'Chromosome Abnormalities and Genetic Counseling', and is presently preparing a 4th edition. He shares a spot in Professor Stephen Robertson's office in the Hercus Building.
Professor Gardner is a semi-retired medical geneticist. He is an Otago graduate, who was previously a member of the Paediatrics Department (1977–1993), before moving to the Genetic Service based at the Royal Children's Hospital in Melbourne (1993–2007). He has broad clincal interests, with a particular focus on inherited cerebellar ataxias and chromosomal disorders. He co-authors the textbook 'Chromosome Abnormalities and Genetic Counseling', and is presently preparing a 4th edition. He shares a spot in Professor Stephen Robertson's office in the Hercus Building.
PhD students
Annika Sjoeholm
PhD student
 Pancreatic insufficiency results from diminished pancreatic enzyme or bicarbonate secretion leading to maldigestion, the clinical hallmark of which is steatorrhoea. In severe cases this can result in failure to thrive, chronic diarrhoea, and other nonspecific gastrointestinal disturbance. Pancreatic insufficiency can occur in both paediatric and adult patients, and can be inherited. Our understanding of these heritable forms is improving as genomic technologies advance. As such it is possible that previously unrecognised isolated enzyme deficiencies may exist.
Pancreatic insufficiency results from diminished pancreatic enzyme or bicarbonate secretion leading to maldigestion, the clinical hallmark of which is steatorrhoea. In severe cases this can result in failure to thrive, chronic diarrhoea, and other nonspecific gastrointestinal disturbance. Pancreatic insufficiency can occur in both paediatric and adult patients, and can be inherited. Our understanding of these heritable forms is improving as genomic technologies advance. As such it is possible that previously unrecognised isolated enzyme deficiencies may exist.
The Clinical Genetics Group at the University of Otago have identified a local whānau with a genetic deficiency of a specific pancreatic enzyme. In the 1000 Genome Project it has been shown that the same gene deletion seen in the local family is present in 4% of the population - this means that the condition we are interested in could be present in 1 in 625 people, and is a potentially unrecognised disease entity. In collaboration with clinical pathologists, as well as local adult / paediatric gastroenterologists and paediatricians, we will seek to identify a cohort of participants with otherwise unexplained pancreatic insufficiency. Via the clinician responsible for the participant, we will invite them to our study to voluntarily provide a DNA sample to identify the genetic mutation. If the genetic mutation of interest is identified, we will invite the participant to give further information on their symptoms as well as a blood sample for other laboratory markers of pancreatic insufficiency (for example micronutrient deficiency), and growth parameters.
Specifically we aim to:
- Identify a cohort of participants with pancreatic insufficiency of unclear aetiology (major causes excluded), and to screen for mutations in genes of interest.
- Characterise the biochemical and clinical presentation of this disorder in this cohort of individuals.
The projected benefits this study provides include the identification of a group of participants who would otherwise have an undiagnosed cause for their pancreatic insufficiency. This may clarify how these genetic mutations might affect growth and other parameters such as micronutrient deficiency and lipid profiles. The investigators view this as an opportunity for the participant to be more informed of their health status, and as a step towards forming a treatment for such participants.
Amy Jones
PhD student
 I completed my BSc (Hons) in 2019 investigating Pseudomonas aeruginosa, the bacteria responsible for the majority of lung infections in cystic fibrosis patients.
I completed my BSc (Hons) in 2019 investigating Pseudomonas aeruginosa, the bacteria responsible for the majority of lung infections in cystic fibrosis patients.
In 2020 I began my PhD in the Clinical Genetics group. My project aims to understand how metabolism contributes to neurodevelopment. Specifically, I will be investigating the metabolite glutamine, one of the most abundant amino acids in the human body. My work utilises genetic and biochemical techniques to understand how glutamine influences neurodevelopment.
Other students
Hayley Gibson
BMedSc(Hons) student
 After completing my BSc in Anatomy and Genetics in 2019, I accepted a position at Otago Medical School and have completed my pre-clinical years of training. With research being an integral part of medical development I decided to do a BMedSc(Hons) and in 2022 I began my research in the Clinical Genetics Group under the supervision of Dr Emma Wade and Prof. Stephen Robertson. My research project is attempting to understand the pathogenesis of a rare genetic disorder, frontometaphyseal dysplasia, which is one of a spectrum of certain skeletal disorders. By using advanced genetic and biochemical technologies such as CRISPR gene editing this project aims to better understand the molecular pathways leading to these diseases as well as build a better foundation of understanding of how the skeletal system develops during embryonic life.
After completing my BSc in Anatomy and Genetics in 2019, I accepted a position at Otago Medical School and have completed my pre-clinical years of training. With research being an integral part of medical development I decided to do a BMedSc(Hons) and in 2022 I began my research in the Clinical Genetics Group under the supervision of Dr Emma Wade and Prof. Stephen Robertson. My research project is attempting to understand the pathogenesis of a rare genetic disorder, frontometaphyseal dysplasia, which is one of a spectrum of certain skeletal disorders. By using advanced genetic and biochemical technologies such as CRISPR gene editing this project aims to better understand the molecular pathways leading to these diseases as well as build a better foundation of understanding of how the skeletal system develops during embryonic life.
Recent photos of the Clinical Genetics Group

2022: Left to right: Back row: Ben Halliday (Postdoctoral Fellow), Stephen Robertson (Group leader), Tim Morgan (Laboratory Technician), Kam Salt (PGDipSci). Front row: Emma Wade (Postdoctoral Fellow), Amy Jones (PhD student), Hayley Gibson (BMedSc(Hons) Student), Elizabeth Goodin (Assistant Research Fellow), Padmini Parthasarathy (Assistant Research Fellow), Zandra Jenkins (Research Fellow).
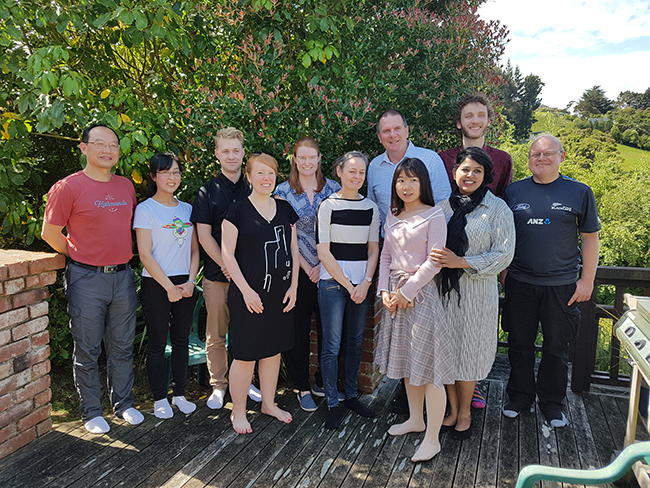
2018: Left to right: Back row: Wenhua Wei (Senior Research Fellow), Kaya Fukushima (Summer Student), Sean Driver (Masters student), Emma Wade (Postdoctoral Fellow), Stephen Robertson (Group leader), Ben Halliday (PhD student), Tim Morgan (Laboratory Technician). Front row: Annika Sjoeholm (PhD student), Zandra Jenkins (Research Fellow), Hui Peng (Visiting PhD Scholar), Padmini Parthasarathy (Assistant Research Fellow).