 Monday 8 January 2018 3:50pm
Monday 8 January 2018 3:50pmServicemen who suffered horrific facial injuries during the two world wars were given new hope as a result of the revolutionary plastic surgery techniques and treatments pioneered by two extraordinary University of Otago men.
During World War One, the founding Dean of the Otago Dental School, Dr H. Percival Pickerill, was part of a team that developed new procedures for skin and bone grafting, higher standards of hygiene to combat infection and new methods of anaesthesia. He and his team treated more than 200 New Zealand, British and other Commonwealth troops injured in the trenches, 59 of whom returned to New Zealand with him to continue their treatment at Dunedin Hospital.
During the next world war, this life-changing work was continued by another Otago alumnus Sir Archibald McIndoe. Treating airmen severely disfigured by exploding aircraft fuel, McIndoe transformed outcomes for his patients, developing many of the principles of burns treatment that are still used today. He introduced saline baths for extensively burnt patients, improving healing times and survival rates. He dramatically advanced tissue transfer techniques: skin grafts were undertaken, noses replaced, eyelids reformed and facial features re-established. However, McIndoe realised that more than physical treatment was required. He also emphasised the importance of the social reintegration of his patients back into normal life, encouraging the formation of the now-famous “Guinea Pig Club”.
Banner: Lieutenant Colonel H.P. Pickerill, Officer Commanding Otago Military Hospitals, 1919, MS-3094/038. Hocken Collections Uare Taoka o Hākena.Today
1
'Cool science' aids dental developments
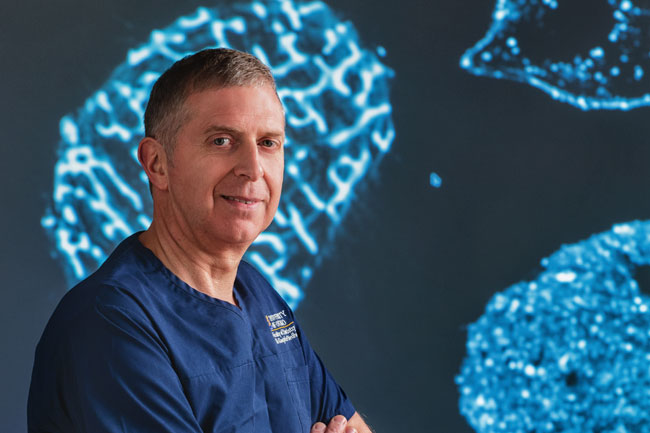
Professor Warwick Duncan: “We're trying to make a new tool to assist diagnosis of gum disease around teeth and dental implants.”
Professor Warwick Duncan, head of Oral Sciences at Otago's Dental School, is working on two significant advances in dental technology that could cut the cost of treatments, improve general health and involve New Zealand's agricultural sector with a new high-value product.
Aside from his University research, Duncan runs a private practice where he experiences problems first hand.
“As a periodontist I treat gum disease, take teeth out and graft bone to be able to implant new teeth as necessary. But as mouths are relatively filthy places, infections can occur and if grafts don't work you can actually lose bone. To a certain extent we can manage that with antibiotics, but we're trying to reduce their use.”
“Both SilverBone and UltraD3 are getting to very exciting stages, with likely results expected in the next couple of years.”
The drive for improvement sees Duncan heading an international and interdisciplinary team including Chemistry's Dr Carla Meledandri and Dr Nina Molteno from Molteno Ophthalmic Ltd, a Dunedin manufacturer specialising in bone graft materials.
“Molteno uses cow bone as the basis of a grafting material in eye sockets and we use it for dental applications. An existing product uses New Zealand beef bones, which are exported to a company in Switzerland where they turn them into grafting material and send that back to us at a high mark-up.
“This doesn't make sense when beef bone is a by-product of our agricultural industry and just goes to make blood and bone instead of being turned into a high-value product. We need to improve upon that material, make it ourselves and get costs down.”
The cost of dental treatment is increasingly important since research revealed significant links between oral and general health.
One of the Otago development team's main challenges is fighting infection, which is particularly prevalent in oral work where there is a higher likelihood of damage from bacteria than in ophthalmic and orthopaedic surgeries. There's also increasing concern about rising bacterial resistance to antibiotics.
Working with manufacturer Molteno and nano-scientist Meledandri, Duncan's team has come up with a new bone-based grafting material, SilverBone, that is robust enough for dental work and contains silver with anti-bacterial properties.
Cell culture work is now fine-tuning the new graft material to balance maximum protection from infection and maximum healthy bone growth.
“It would be nice not to have animal testing phases, but we have to show it is safe and promotes new, healthy bone growth. So now we are working on observations in the chemistry laboratories to create something that will be superior and save money and be sold and used in dental procedures every day.”
Duncan is also working on developing UltraD3 – a miniaturised ultrasound device to help with dental diagnosis – with Callaghan Innovation engineer Paul Harris and a world-leading team with capabilities in dental research, ultrasonics, electronics and materials science.
“We're trying to make a new tool to assist diagnosis of gum disease around teeth and dental implants. When Paul first asked how I diagnose gum disease I told him I poked it with a stick. It's actually called a periodontal probe, but it's much the same thing. We're aiming to do better than that.”
The diagnostic technique hasn't changed for a century, so it's high time for an improvement, says Duncan.
Gum disease affects one in three adult New Zealanders and is the world's sixth most prevalent condition, with strong links to diseases with high morbidity and mortality. Early intervention should reduce both discomfort and late stage treatments, save money and improve health.
Ultrasound is used for many conditions, such as in breast cancer diagnostics, where it measures changes in tissue stiffness.
“The challenge is to make the device small enough to fit comfortably in the mouth and accurate enough dealing with very small amounts of tissue. We're now on version three and we're getting close. It should be a very useful diagnostic device and almost certainly will be able to be used in other ways in the future.
“Both SilverBone and UltraD3 are getting to very exciting stages, with likely results expected in the next couple of years. It's really cool science and it's really enjoyable.”
Funding
Ministry of Business, Innovation and Employment
2
3D-bioprinting breakthrough

Dr Khoon Lim and Associate Professor Tim Woodfield: They came up with a clever “little chemical formula” for a range of bio-inks that could be cured by visible light…
Christchurch researchers have patented a special “bio-ink” that is putting them at the forefront of international research into the 3D-bioprinting of living human cartilage, tissue and bone.
The ability to 3D-print human cells that survive and thrive inside the body is the aim of teams of regenerative medicine experts around the world. Researchers from the University of Otago's Christchurch Regenerative Medicine and Tissue Engineering (CReaTE) group are focused on producing large and viable pieces of complex human tissue, bone and cartilage created from a patient's own cells, for implantation by orthopaedic surgeons.
Dr Khoon Lim trained as an engineer and now works with a growing team of biomedical experts and other engineers at the University of Otago, Christchurch campus. With CReaTE director Associate Professor Tim Woodfield, Lim is focused on perfecting the bio-inks that are crucial to successful 3D-bioprinting in orthopaedics.
A study found that 3D-bioprinting with the CReaTE bio-inks resulted in at least a third more cells surviving the printing and hardening process.
Bio-inks are gel-like substances that carry human cells as they are 3D-printed, then set into the required shape. They need to support cell growth and, once transplanted into the body, biodegrade, says Lim.

Because bio-inks are in liquid form, they need to be “cured' or hardened into the shape required. This stage, explains Lim, is the part of the 3D-bioprinting process most damaging to cells.
“A lot of research groups have hardened the bio-inks by exposing them to UV rays. UV rays are the part of the sun that damages our skin and gives us sunburn, so you can imagine that they would not be great for the precious cells we want to survive and be in optimum condition when we put them inside the body to grow.''
Lim and Woodfield came up with a clever “little chemical formula” for a range of bio-inks that could be cured by visible light (what we humans can see) rather than the invisible and damaging UV light. Their idea worked.
A study found that 3D-bioprinting with the CReaTE bio-inks resulted in at least a third more cells surviving the printing and hardening process. As well as being kinder to cells, CReaTE's bio-inks are also able to be adapted for different printing requirements.
As Lim explains, 3D-bioprinters come in different types and scientists use them to print different types of tissues. Just as normal printers come with their own dedicated cartridges, most bio-inks are designed specifically for certain types of 3D-bioprinter. The CReaTE bio-inks are compatible with many different 3D-bioprinters, and can be combined or printed in layers to produce complex, functional tissue.
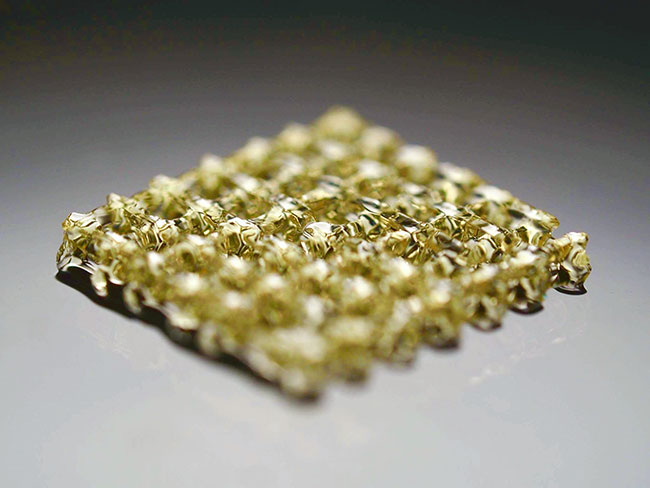
The technology and invention have been patented by Otago Innovation Limited, the University of Otago's commercialisation company. Further research is being conducted to 3D-bioprint functional bone, cartilage and blood vessels.
Lim says he and Woodfield hope that eventually their invention might be used in laboratories around the world to produce living tissue and benefits to patients.
Funding
Rutherford Discovery Fellowship
Health Research Council
MedTech CoRE
Canterbury Medical Research Foundation
Marsden Fund
3
Depression detection
THE BCI team: “So, we are looking at people – some of whom seem 'depressed' and others seem 'not depressed' – and asking the machine to separate them on their brain activity.”
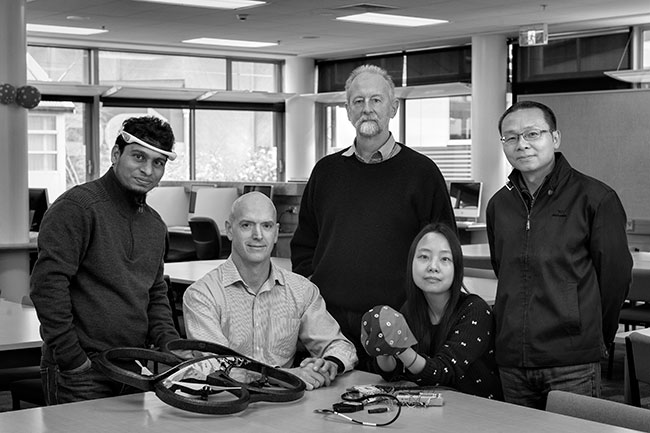
A collaboration between psychology and computer science researchers at Otago is seeking to use what is called brain-computer interface technology (BCI) to identify and potentially treat depression.
The research team comprises Professor Neil McNaughton and Dr Shabah Shadli (Psychology), together with Associate Professor Zhiyi Huang, Associate Professor Brendan McCane and PhD student Shenghuan Zhang (Computer Science).
The researchers explain that depression affects millions of people worldwide and costs billions of dollars each year, yet the biological basis of depression is largely unknown and clinical diagnosis is based on symptoms rather than underlying causes.
“If it is truly the brain activity that determines whether the person has the problem, maybe we can train them to do the opposite and maybe they will get well.”
Their work involves recording the brain's electrical activity in volunteers wearing caps fitted with electrodes. McNaughton says that this information is fed into “machine learning” computer systems that McCane is building, which look for patterns that link to depressive personality.
“We presume that mental disorders have some sort of cause in the brain and that different causes will look different,” McNaughton says. “So, we are looking at people – some of whom seem 'depressed' and others seem 'not depressed' – and asking the machine to separate them on their brain activity. We hope to find in that brain activity biomarkers or characteristic patterns and prove the patterns are specific to depression.
“We are not looking for somebody who is currently feeling depressed, because anybody can feel depressed momentarily. The key thing we are looking for is a personality trait that, when it is extreme, means that the person has a good chance of being diagnosed as having a major depressive disorder.”
McNaughton says that this could lead to exciting new treatments. “If it is truly the brain activity that determines whether the person has the problem, maybe we can train them to do the opposite and maybe they will get well.”
He says that the training would involve connecting a person's brain via a headset to a computer. This would work like a drone control system already developed by Huang.
“Instead of controlling a drone, when their brain activity looks depressive, this would move an object on the computer screen and they would try to learn to move it back to change that brain state.”
McNaughton adds that, if the techniques work with depression, they should also work with many other psychiatric conditions.
Funding
EEGSmart, China
University of Otago
4
The full picture
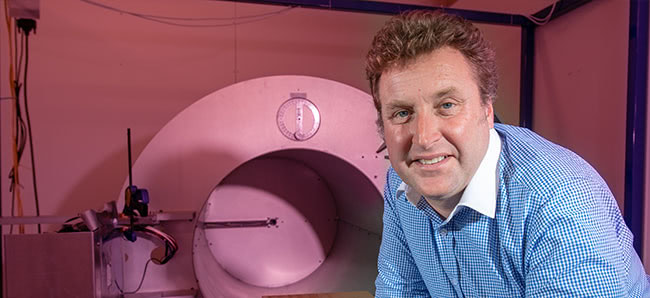
Professor Anthony Butler: “X-ray spectral information allows health professionals to measure the different components of body parts such as fat, water, calcium and disease markers.”
A new medical scanner incorporating world-leading technology is set to revolutionise the diagnosis and treatment of diseases such as cancer and heart disease, saving millions of lives.
University of Otago, Christchurch Professor Anthony Butler invented the MARS scanner with his father, Professor Phil Butler of the University of Canterbury, adapting technology being used by the European Organization for Nuclear Research (CERN) in the hunt for the “God particle”.
Thirteen years in development, the Butlers' scanner produces images with significantly improved diagnostic information, measuring the x-ray spectrum to produce colour images (instead of black and white). However, it is the use of CERN's Medipix3 technology that sets their machine apart: with smaller pixels and accurate energy resolution, it produces 8,000 times more data than CT or MRI scans, allowing an unprecedented and non-invasive view inside the human body.
“After more than a decade of intense research and development, it is really exciting to have reached a point where it's clear the technology can be used for routine patient care.”
In 2018, the first human was scanned by the MARS technology. The resulting images captivated media and research groups around the world, with scores of global media outlets reporting on the paradigm-shifting invention and millions of Twitter users viewing the startlingly-clear images of inside a human wrist and ankle.
The Butlers and their growing research team are now undertaking clinical trials involving Christchurch orthopaedic and rheumatology patients. They are scanning these patients with their technology, and comparing this with the best CT scanner currently on the market to illustrate how MARS produces superior images and its ability to diagnose conditions such as the deterioration of bone or cartilage.
“Traditional black and white x-rays only allow measurement of the density and shape of an object,” Butler says. “X-ray spectral information allows health professionals to measure the different components of body parts such as fat, water, calcium and disease markers.
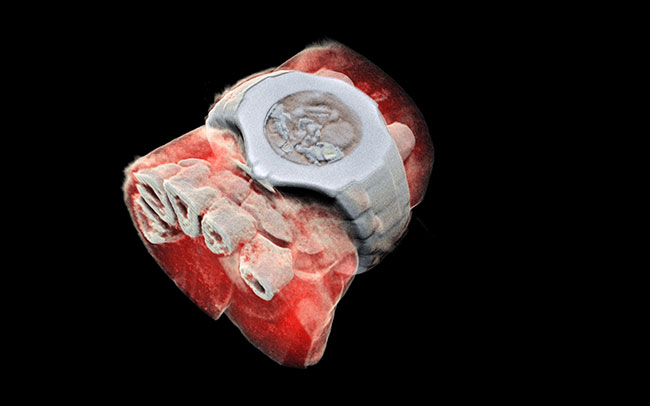
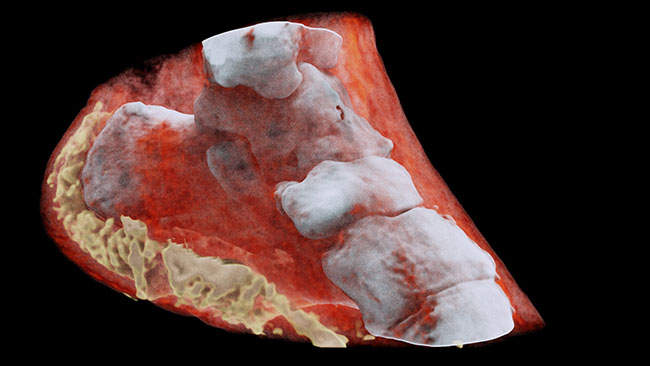
“So far, researchers have been using a small version of the MARS scanner to study cancer, bone and joint health, and vascular diseases that cause heart attacks and strokes. In all of these studies, promising early results suggest that when spectral imaging is routinely used in clinics it will enable more accurate diagnosis and personalisation of treatment."
More clinical trials are needed, but the research team hopes to have a commercial version of the scanner available for point-of-care use within the next two to three years.
Butler says he is humbled and immensely satisfied his invention could save millions of lives by enabling diseases to be diagnosed faster and more accurately.
“After more than a decade of intense research and development, it is really exciting to have reached a point where it's clear the technology can be used for routine patient care.”
Funding
University of Otago
University of Canterbury
Ministry of Business, Innovation and Employment
MARS Bioimaging Ltd
GE Healthcare
