Expertise informs action
The COVID-19 global pandemic has dominated 2020, its impact defined by the strengths – and weaknesses – of individual national responses. Here at Otago, we are proud of our experts' responses to this rapidly-changing situation. They have risen to the challenge and have had a fundamental influence on the New Zealand government's decision-making – and continue to do so.
A rapid response
As reports of a new coronavirus emerged from Wuhan in China, epidemiologists at the University of Otago and internationally feared that this was the pandemic they had long been predicting.
As the crisis unfolded, governments around the world were placed under severe pressure to mount an effective response. Here in New Zealand, dozens of experienced public health and infectious diseases researchers from the University of Otago – together with others from across the country – were able to provide expertise to inform our national public health policy, from early warnings to first responses, and to building capacity to contain the epidemic. Their influence extended across television, radio, print media and online forums, with many featuring internationally.

Professor Philip Hill
Otago's Professor Philip Hill, inaugural holder of the McAuley Chair in International Health, co-director of Otago's Centre for International Health and chair of Otago's Infectious Disease Emergency Planning Group, says New Zealand was not well prepared for COVID-19.
“The country was not ready and the pandemic challenged the part of our health system that had become our weakest. The only pandemic plan we had was mainly based around the influenza virus – but the new virus was not an influenza virus.”
Hill – who has been appointed to the advisory committee to oversee the implementation of the New Zealand COVID-19 Surveillance Plan and Testing Strategy – was just one of many Otago researchers who saw problems early and tried to contribute to solutions.
“Rather than just listen to what the Chinese were saying, it was important to take note of what they were actually doing. For example, setting out to build a huge hospital in 15 days in Wuhan meant that they were in serious trouble. But by late February it became clear that China was actually gaining control over the virus,” he says. “Their public health approach had been huge, sophisticated, tailored and integrated.”
It also became clear that some other Asian countries were succeeding in controlling even large outbreaks, including those that featured community transmission. Hill, Wellington-based infectious diseases physician Dr Ayesha Verrall and others realised that those countries had one intervention in common – rapid case contact management.
Verrall began lobbying for a rapid scaling-up of testing and contact tracing, and was commissioned to audit the government's existing contact tracing methods and to recommend ways to improve systems and scale them up. Within six weeks her recommendations were in place.
Internationally-recognised epidemiologist and public health physician Emeritus Professor Sir David Skegg “entered the fray at just the right time”, says Hill. He warned the government's Epidemic Response Committee that failing to improve New Zealand's contact tracing system would be like playing Russian roulette with the health of the population. Skegg also repeatedly highlighted the urgency of widespread testing – within the community and at the border: “There is no such thing as over-testing and every day counts”.

Professsor Michael Baker and Professor Nick Wilson
Scientific advice changed as more was learned about the virus. From early February, the University of Otago Wellington's (UOW) Professor Michael Baker and Professor Nick Wilson urged the government to ramp up its response by preparing the population for a massive upgrade in protective practices, strengthening border controls and improving quarantine procedures. They were the first to alert the government to how many New Zealanders might die if officials made the wrong calls.
“In early February we warned that the pandemic could get very bad. But it became much easier to convince officials of the urgency to act because of what was happening in Italy, which was struggling with the pandemic despite having better hospital capacity and more ICUs per population than New Zealand,” says Wilson. “If our government had delayed by just another week we could have lost control.”
In March their Health, Environment and Infection Research Unit (HEIRU) team estimated 8,600 to 14,400 deaths as being plausible if there were inadequate controls. The worst-case scenario – letting the virus run its course through the population without intervention – had suggested a death toll of 28,000.
Initial lockdown followed the influenza pandemic plan and aimed at mitigation – trying to slow down the spread of the virus to avoid overloading the unprepared health system with patients. But modelling by Wilson and Baker soon showed that lockdown provided a real chance to eliminate (not eradicate) community transmission of the virus in New Zealand. With their UOW colleagues they wrote the world's first COVID-19 elimination strategy and published it in the New Zealand Medical Journal on 3 April 2020, an approach ultimately adopted by the New Zealand government. They also published an article on the New Zealand response and initial success with COVID-19 elimination in the New England Journal of Medicine, regarded as the world's highest impact medical journal. nejm.org/doi/full/10.1056/NEJMc2025203
Throughout the crisis – including after COVID-19 was successfully eliminated and then later reappearing in an outbreak in Auckland – the researchers have continued to advocate for the wearing of face masks in appropriate settings, for improved contact tracing with digital tools, for a cautious science-based approach to border management (including quarantine) and for the need to plan for the introduction of a vaccine. They have also recommended major changes to the way public health services are organised – such as a new national public health agency for disease prevention and control – and have urged the government to launch an inquiry into its response to the pandemic to identify ways it can be improved.
"We need to learn from the COVID-19 response as there are other threats on the horizon that are far more destructive for all of us,” says Baker.
At a glance
From early February to late September 2020 dozens of academics from across Otago's campuses made a substantial contribution to the COVID-19 debate, here in New Zealand and around the world.
New Zealand
Over 300 TV appearances
Over 900 radio interviews
Over 2,900 newspaper articles
Over 9,500 pieces of online news
Global
Nearly 7,000 international media hits
Over 1 million social media interactions
Aggregate readership of potentially 24 billion across five continents
COVID captured

Professor Miguel Quiñones-Mateu

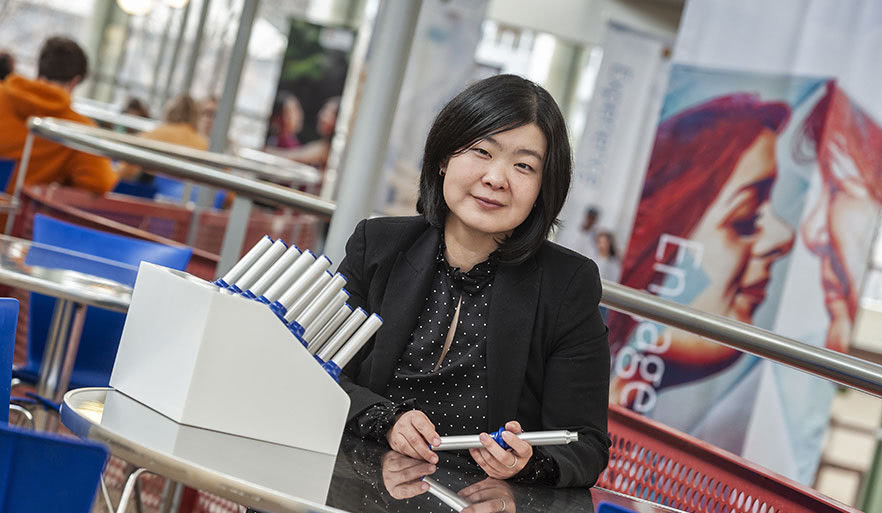
Dr Jemma Geoghegan
As Otago's epidemiologists informed the government's public health response, the University's infectious diseases scientists were also hard at work. Professor Miguel Quiñones-Mateu and Associate Professor James Ussher (Microbiology and Immunology) developed a diagnostic test for COVID-19 in their Dunedin laboratories just as the first case was detected in the southern region.
Once the test was up and running, their priority shifted to providing samples of the virus for culture and genetic sequencing. Quiñones-Mateu, who holds the Webster family Chair of Viral Pathogenesis, says it took just 36 hours to sequence the full genome of the viruses collected from the first two patients.
“Having the virus opens the door to doing so many different things. We now have more than 30 different projects people want to do with us because we have the virus here. I'm talking about diagnostics methods, disinfection of PPE, vaccine development and antivirals.”
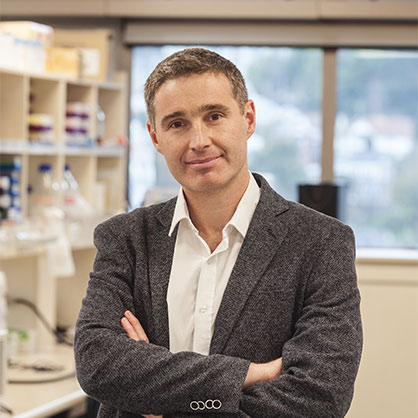
Associate Professor James Ussher
Although there have been no major mutations in the virus, there are several distinct clusters circulating in different parts of the world. “It is important for us to know which virus is circulating here in New Zealand,” says Quiñones-Mateu. “Some came from Europe, some came from China, others from the US. So we need to keep an eye on any virus we have here.”
Evolutionary virologist Dr Jemma Geoghegan (Microbiology and Immunology) is heading a nationwide group involving ESR (Institute of Environmental Science and Research)and other universities using genomic sequencing to track how the virus came into New Zealand and how it worked its way through the country.
Geoghegan says genomes can provide insights that epidemiological data cannot – and in real time. “We can help link a case to a cluster to which there is no apparent epidemiological link: by using the genome we can link that sample to a known cluster or exclude it from a cluster.”
This sort of information has proven invaluable in the resurgence of the virus in South Auckland, enabling policy-makers to link cases to a known cluster, to measure the effectiveness of lockdown measures and, by looking for any genomic diversity, seeing whether or not there is undetected community transmission.
Vaccine development
The University of Otago is part of a nationwide alliance to secure a vaccine for New Zealand – Vaccine Alliance Aotearoa New Zealand – Ohu Kaupare Huaketo (VAANZ)– working with a number of research groups, institutions and companies around the country, including the Malaghan Institute of Medical Research, Victoria University of Wellington, AgResearch, Avalia Immunotherapies, ESR and South Pacific Sera.
Three main candidates are being pursued, with Quiñones-Mateu's team leading work on an inactivated viral vaccine candidate. Another is a recombinant spike protein vaccine being developed at Victoria University of Wellington, and the third is a pan-coronavirus vaccine being explored by Avalia Immunotherapies with international collaborators.
Ussher, who is VAANZ's science director, says Otago is also a key partner in developing a pipeline for evaluating vaccines. The SARS-CoV-2 strains isolated in the University's PC3 lab will be used in a preclinical challenge model and to measure antibody responses following vaccination, to see if they are capable of blocking infection. A strategy is also being developed for second generation vaccines in case the virus mutates and for any future coronaviruses that may emerge.
“We're trying to stay one step ahead of the virus by having vaccine candidates that are ready to go and could just be taken off the shelf and slotted straight into a vaccine development programme,” he says.
Doing the detail
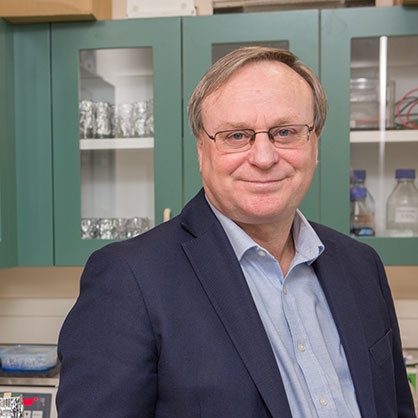
Professor Vernon Ward
Teams led by virologist Professor Vernon Ward (Microbiology and Immunology) and structural biologist Professor Kurt Krause (Biochemistry) are also drawing on their extensive experience and expertise to find ways to beat SARS-CoV2, the virus that causes COVID-19.
Ward's laboratory is working with renowned medicinal chemist Professor Dame Margaret Brimble (University of Auckland) to identify potential antiviral drug targets for which her lab can create compounds to form the basis of new drugs.
But, he warns, it is likely multiple drugs will be needed for efficacy and because it is often easy for resistance to develop to a single drug.
“So the question is – will there be a magic bullet come out of existing compounds or do we need to develop specific targeted compounds? I suspect it is both. We will find drugs that help and new drugs will be needed in combination as they become available.”
Ward is already leading the MBIE-funded New Frontiers in Antiviral Development project (see Otago Magazine issue 50) and has started a project looking at 3CLpro protease of SARS-CoV2.
“We're taking the approach that sooner or later there is a reasonable chance we will need to have something specifically designed for this virus, rather than repurposed from something else.”
Professor Kurt Krause
They will also undertake a longer-term project focusing on the polymerase looking at different approaches to targeting how the virus replicates its genome.
Once they have a likely target and compound to use on it, they turn it over to Krause and his lab to evaluate, using X-ray crystallography.
This technique allows them to examine these viral proteins at an atomic level to see how well the antiviral compounds bind to them. They can then understand how to improve them so they can do an even better job of blocking the virus from functioning.
“Margaret Brimble has an international reputation for her creative synthetic chemistry and her ability to synthesise proteins and peptides, so Vernon's and my lab will be testing them and feeding back into her work with any suggestions that we have,” says Krause.