What are temporomandibular disorders (TMDs)?
TMDs are a group of conditions that cause pain and dysfunction in the jaw region. Specifically, TMD is defined by:
Simply the presence of non-painful joint noises is NOT a TMD. 60% of people have non-painful joint noise such as clicking and popping, which is considered normal. If there is NO pain nor dysfunction, then it is unlikely a TMD.
The most common symptoms of TMD are pain (jaw tenderness, headaches, earaches, facial pain) and jaw dysfunction (decreased mouth opening, abnormal jaw movement when opening). However, people with TMD can also experience a wide range of symptoms affecting the head and neck regions (Figure 1). Below the figure we have also provided a text list of the (List 1). symptoms.
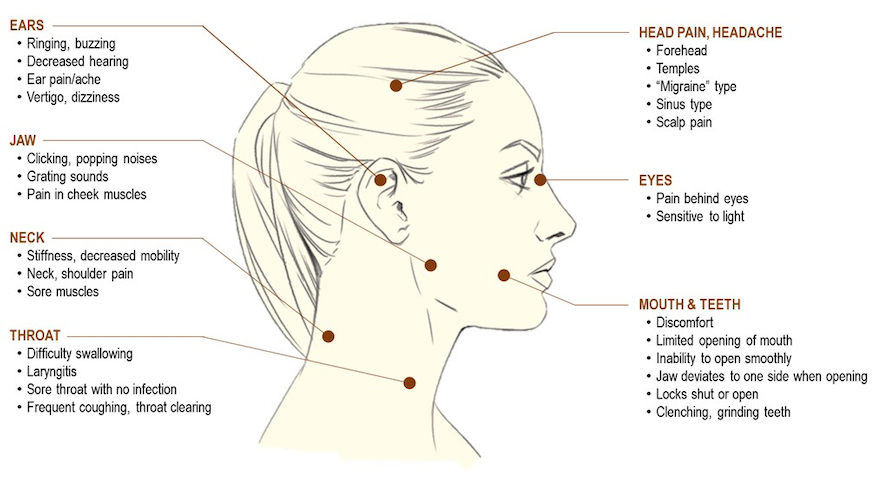
Figure 1. Symptoms of TMD
List 1: Symptoms of TMD:
Ears: Ringing, buzzing. Decreased hearing. Ear pain/ache. Vertigo, dizziness
Jaw: Clicking, popping noises. Grating sounds. Pain in cheek muscles.
Neck: Stiffness, decreased mobility. Neck, shoulder pain. Sore muscles.
Throat: Difficulty swallowing. Laryngitis. Sore throat with no infection. Frequent coughing, throat clearing.
Head pain, Headache: Forehead. Temples. "Migraine" type. Sinus type. Scalp pain.
Eyes: Pain behind eyes. Sensitive to light.
Mouth and teeth: Discomfort. Limited opening of mouth. Inability to open smoothly. Jaw deviates to one side when opening. Locks shut or open. Clenching, grinding teeth.
Is it called temporomandibular joint (TMJ) or TMD?
Many people use the terms TMJ and TMD interchangeably. The TMJ is a unique joint in the body that opens/closes the mouth (Figure 2). People sometimes refer to problems in the jaw region simply as 'TMJ'. However, not all jaw problems come from the TMJ, so conditions that cause pain and/or dysfunction in the jaw region are called 'TMD'.
What is the temporomandibular joint (TMJ)?
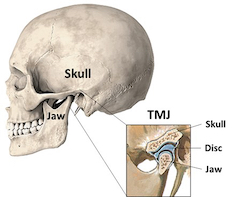
The TMJ is a unique joint on either side of the face that moves the jaw to allow opening/closing of the mouth. The TMJ connects the jaw to the skull with a disc in between the two bones. This disc helps the jaw move in different directions and is usually the cause of normal, non-painful joint sounds during movement such as click and popping.
Figure 2. Temporomandibular joint (TMJ)
Who develops TMD and what causes it?
Although anyone can develop a TMD, the vast majority are women between the ages of puberty and menopause. Although records suggest up to 12% of people will have a TMD, this is likely an underestimate as many people go undiagnosed.
Causes of TMD have been linked to:
- Injuries to the face/jaw (i.e., blunt trauma, fracture, etc.)
- Excessive or long mouth opening (i.e., dental procedures)
- Diseases such as inflammatory arthritis.
- Chronic pain – chronic TMD that lasts longer than 3 months is classified as a chronic pain disorder.
How is TMD diagnosed and how is it treated?
TMD is usually diagnosed by first ruling out other possible causes for jaw pain and dysfunction, such as infection or tooth problems. Scans such as an x-ray or MRI may be performed if the problem is thought to be inside the TMJ (i.e., fracture or arthritis). Clinicians may conduct a physical exam, to see how your jaw moves, feel surrounding muscles, and look inside your mouth.
In New Zealand, the most common clinicians that see people with TMDs are general medical doctors, dentists, and physiotherapists. In some cases, referral to a specialist, such as a surgeon, may be needed if there are severe structural problems in the TMJ.
There are many ways to relieve TMD symptoms. Depending on what is causing your problem, your provider may advise the following treatments:
- Specific jaw exercises
- Massage
- Acupuncture
- Medication: Pain relievers may help ease the pain of some types of TMD in the short term. Non-steroidal anti-inflammatory drugs (NSAIDs) such as Nurofen/ibuprofen are usually recommended. Certain types of antidepressant medicines, including tricyclic antidepressants, have been shown to relieve pain in people with TMD.
- Mouthguard (also known as a mouth splint or night guard): Decreasing night-time jaw clenching and teeth grinding, a mouthguard may ease the tension in your jaw muscles.
- Stress management: managing stress and anxiety is important if this is causing or contributing to the pain. There are several ways to help relieve stress, including regular exercise, yoga, deep breathing exercises, and meditation.
What is the outlook (prognosis)?
Generally, the outlook is good. Most TMDs improve over time and do not become worse. It is very rare to have any complications with this condition. Some people do have symptoms that last longer or come back (recur). However, even these can usually be improved with the treatments described above. Most people do not need more invasive treatment or surgery and will get better over time with conservative treatments.
Further information:
This information page is provided as part of a programme of work lead by Dr Carrie Falling. If you would like some information about the research carrie.falling@otago.ac.nz