4.1. Overview of Module 4
In this module you will learn about the various roles of vitamin C in the prevention and treatment of cancer. The background for the initial controversy around vitamin C in cancer therapy will be clarified. The mechanisms of action specific to cancer will be highlighted. The use of both oral and intravenous vitamin C in relation to cancer will be discussed.
Following completion of this module the participant will be able to:
- Discuss the evidence-based role of vitamin C in cancer prevention and therapy to colleagues and patients (Communication, Scholarship, Professionalism)
- Explain the rationale for oral versus intravenous vitamin C use in cancer to colleagues and patients (Communication, Scholarship, Professionalism)
- Describe the different ways vitamin C works in cancer to colleagues and patients (Communication, Scholarship, Professionalism)
- Assess the potential usefulness of vitamin C administration to patients with cancer in their healthcare practice (Management)
- Apply knowledge on vitamin C administration to patients with cancer in their healthcare practice, including any safety issues to be aware of (Clinical expertise)
Length of activity: 55 min (25 min reading + 30 min activity)
RNZCGP Endorsed: 0.9 CME credit
CICM Accredited: 0.9 point
4.2. Vitamin C status of people with cancer
Many observational studies have consistently shown that patients with cancer have lower mean plasma vitamin C status than healthy controls, and a large proportion of them present with hypovitaminosis C (<23 mmol/L) and outright deficiency (<11 mmol/L) (see figure below and Table 1 in further reading). Severity of the disease appears to impact on vitamin C status, e.g. the proportion of lymphoma patients with hypovitaminosis C was significantly elevated for those with high-burden disease. Patients with higher stage breast and cervical cancers had significantly lower vitamin C status than patients with lower stage disease.
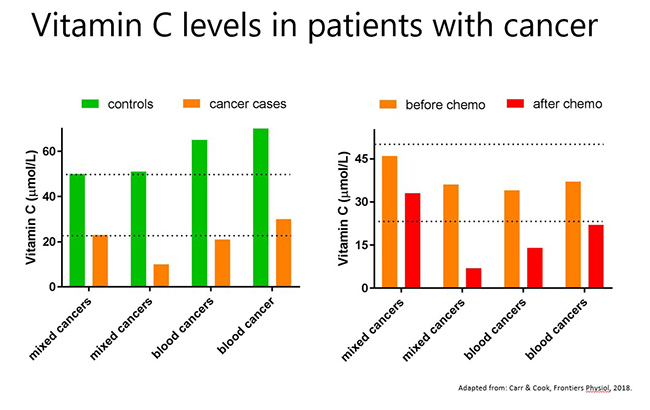
There is also evidence that adjunctive cancer therapies may impact negatively on vitamin C status (see figure above and Table 2 in further reading). It has been noted that administration of some anticancer therapies (such as cisplatin, fluorouracil, nilotinib, and interleukin-2) can significantly lower the vitamin C status of oncology patients and result in scurvy-like symptoms in some cases. Chemotherapy drugs such as cisplatin are known to generate off-target oxidative stress which could contribute to the depletion of vitamin C. Discontinuation of the chemotherapy or administration of supplemental vitamin C to these patients resolved the deficiency.
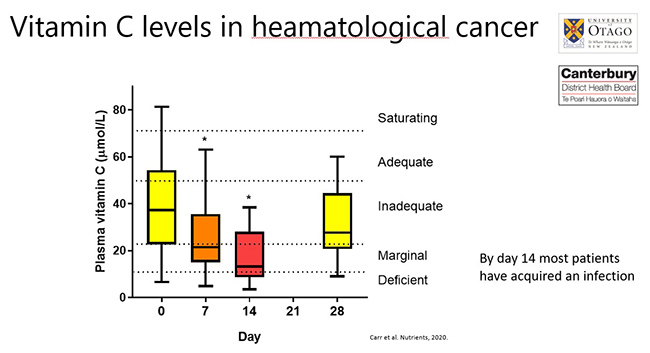
Patients with hematopoietic cancers typically undergo conditioning with multiple chemotherapy agents and a number of studies have shown significantly lower vitamin C status following the conditioning regimens (see figure below). The lowest levels of vitamin C coincide with febrile neutropenia (infection and fever due to low leukocyte counts). Although plasma vitamin C levels appear to return to baseline values approximately one month following chemotherapy, these values are still inadequate.
Of note, administration of IV vitamin C to oncology patients results in lower circulating vitamin C levels compared with administration of the same amount to healthy controls. The finding that oncology patients have a higher requirement for vitamin C is thought to indicate a lower body pool and/or the higher oxidative and pro-inflammatory status of these patients (as indicated by elevated lipid oxidation products or C-reactive protein concentrations). It is interesting to note that animals that can synthesise their own vitamin C in their livers increase their endogenous vitamin C levels when under a tumour burden suggesting enhanced requirements for the vitamin.
Further reading:
-
Intravenous vitamin C for cancer therapy - Identifying the current gaps in our knowledge. Carr and Cook. Front Physiol. 2018.
This review collates the observational studies that have investigated vitamin C status in oncology patients, including the effects of chemotherapy on vitamin C status. -
Patients undergoing myeloablative chemotherapy and hematopoietic stem cell transplantation exhibit depleted vitamin C status in association with febrile neutropenia. Carr et al. Nutrients. 2020.
Our observational study showed significantly depleted vitamin C status in HSCT patients following myeloablative chemotherapy and febrile neutropenia.
4.3. Vitamin C intake/status and cancer epidemiology
4.3.1. Vitamin C and cancer risk
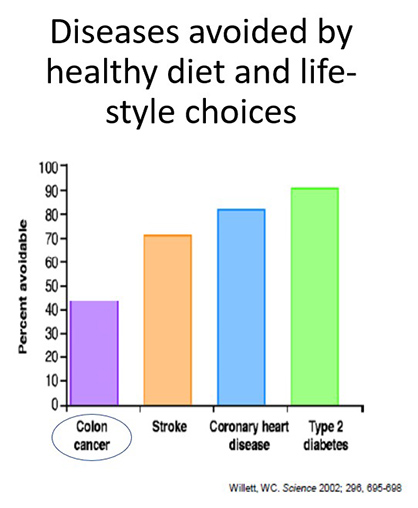 The Global Burden of Disease project has highlighted the most common cancers globally as: skin, respiratory, prostate, breast and colorectal. Research has indicated that some cancers, e.g. colon cancer, can be nearly 50% avoidable with healthy diet and lifestyle choices (see figure below).
The Global Burden of Disease project has highlighted the most common cancers globally as: skin, respiratory, prostate, breast and colorectal. Research has indicated that some cancers, e.g. colon cancer, can be nearly 50% avoidable with healthy diet and lifestyle choices (see figure below).
Most studies have focused on the associations between dietary intakes of vitamin C and specific cancer types; fewer have focused on associations with plasma vitamin C concentrations. Below are examples from meta-analyses (2011-2022).
Total cancers: A meta-analysis of prospective studies has indicated that the relative risk for total cancers per 100 mg/day increment of dietary vitamin C intake was 0.93 (95% CI: 0.87, 0.99, n = 8) and the relative risk per 50 μmol/L increase in blood concentrations of vitamin C was 0.74 (95% CI: 0.66, 0.82, n = 5) (see further reading below).
Gastric cancer: For gastric cancer, each 20 μmol/L increase in plasma vitamin C was associated with a 14% decrease in risk (HR: 0.86; 95% CI: 0.76, 0.96; n = 3). Compared with individuals with plasma vitamin C concentrations ≤28 μmol/L, those with concentrations >28 μmol/L had a 27% reduced risk of gastric adenoma (HR: 0.73; 95% CI: 0.56, 0.94).
Breast cancer: Recent meta-analysis of the association between vitamin C intake and breast cancer risk indicated that the highest versus lowest vitamin C intake was significantly associated with a lower risk of breast cancer (RR 0.86; 95% CI: 0.81, 0.92; n = 54).
Reproductive tract cancers: Vitamin C intake was significantly associated with a reduced risk of cervical neoplasia (OR = 0.58; 95% CI: 0.44 to 0.75; n = 12), and increasing vitamin C intake by 50 mg/day was related to an odds ratio of 0.92 (95% CI: 0.89 to 0.94). However, no significant association between vitamin C intake and risk of ovarian was observed. The relative risk of prostate cancer for the highest versus lowest categories of dietary vitamin C intake was 0.89 (95% CI: 0.83, 0.94; n = 18), with a 150 mg/day dietary vitamin C intake conferring a RR of 0.91 (95% CI: 0.84, 0.98).
Lung cancer: The highest vitamin C intake versus lowest intake was associated with a decreased risk of lung cancer (RR 0.83; 95% CI: 0.73, 0.94; n = 21), with a dose-response relationship indicating the risk of lung cancer decreasing by 7% for every 100 mg/day increase in vitamin C intake.
Digestive tract cancers: Comparing the highest versus lowest categories of vitamin C intake, vitamin C was found to be inversely associated with the risk of oesophageal cancer (OR 0.58; 95% CI: 0.49, 0.68; n = 20), with a linear dose-response relationship indicating an increase in dietary vitamin C intake of 50 mg/day decreasing the risk of oesophageal cancer by 13%. For gastric cancer, every 100 mg/day increment of vitamin C conferred an OR of 0.78 (95% CI: 0.67, 0.90). When comparing the highest with the lowest categories of vitamin C intake, the relative risk for pancreatic cancer was 0.66 (95% CI: 0.58, 0.75; n = 20 case-control and cohort studies). Meta-analysis of 13 cohort studies has indicated that total vitamin C intake (dietary plus supplements) was associated with a decreased risk of colon cancer RR 0.81 (0.71-0.92) for >600 vs. ≤ 100 mg/day.
Urinary tract cancers: The highest vs lowest vitamin C intake was associated with a lower risk of renal cell carcinoma (RR 0.78; 95% CI: 0.69, 0.87; n = 10). In contrast, no significant association between vitamin C intake and risk of bladder cancer has been observed.
Brain cancer: Finally, vitamin C intake was associated with lower glioma risk (RR 0.86; 95% CI: 0.75, 0.99; n = 15).
Currently, there is no evidence from RCTs to support vitamin C supplementation in preventing cancer, keeping in mind the multiple limitations of nutrient RCTs that you learnt about in Module 2. Therefore, vitamin C is often considered to be simply a marker of fruit and vegetable intake. However, because of the pleiotropic functions of vitamin C within the body, including integral roles in various anti-cancer mechanisms, optimising its levels in the body through diet and supplementation may help to reduce the modifiable component of cancer mortality and risk.
In support of this premise, studies in a vitamin C-requiring mouse model indicate that oral vitamin C supplementation of these animals can impair the development of tumours and can also increase the rejection rate of implanted tumour cells. Furthermore, mice that can synthesise their own vitamin C will increase synthesis of the vitamin following xenograft. These all suggest important roles for vitamin C in host defense against cancer.
4.3.2. Vitamin C and cancer mortality
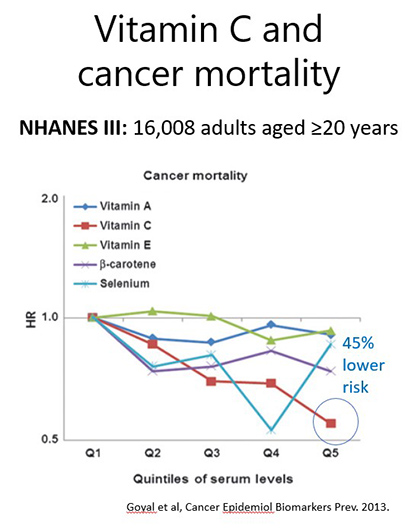 The Global Burden of Disease research indicates that cancer is one of the five leading causes of mortality worldwide. For breast cancer-specific mortality, for example, meta-analysis of the association between vitamin C intake and breast cancer mortality indicated that the highest versus lowest vitamin C intake was significantly associated with lower breast cancer-specific mortality (RR 0.78; 95% CI: 0.82, 0.96; n = 15). An earlier meta-analysis indicated that for breast cancer-specific mortality, the relative risk for a 100 mg/day increase in dietary vitamin C intake was RR 0.78 (95% CI: 0.64, -0.94, n = 7). As we have seen in other modules, vitamin C status may be a more accurate predictor than dietary intake. Analysis of US NHANES data indicated a dose-response decrease in cancer mortality risk with higher vitamin C concentrations (HR 0.55; 0.39–0.79; ≥60 µmol/L vs ≤15 µmol/L serum vitamin C; see figure below).
The Global Burden of Disease research indicates that cancer is one of the five leading causes of mortality worldwide. For breast cancer-specific mortality, for example, meta-analysis of the association between vitamin C intake and breast cancer mortality indicated that the highest versus lowest vitamin C intake was significantly associated with lower breast cancer-specific mortality (RR 0.78; 95% CI: 0.82, 0.96; n = 15). An earlier meta-analysis indicated that for breast cancer-specific mortality, the relative risk for a 100 mg/day increase in dietary vitamin C intake was RR 0.78 (95% CI: 0.64, -0.94, n = 7). As we have seen in other modules, vitamin C status may be a more accurate predictor than dietary intake. Analysis of US NHANES data indicated a dose-response decrease in cancer mortality risk with higher vitamin C concentrations (HR 0.55; 0.39–0.79; ≥60 µmol/L vs ≤15 µmol/L serum vitamin C; see figure below).
Further reading:
-
Dietary intake and blood concentrations of antioxidants and the risk of cardiovascular disease, total cancer, and all-cause mortality: a systematic review and dose-response meta-analysis of prospective studies. Aune et al. Am J Clin Nutr, 2018.
A comprehensive meta-analysis that compared the risk of cancer relative to both dietary vitamin C intake and plasma concentrations. -
Vitamin C Intake and Cancers: An Umbrella Review. Chen et al. Front Nutr. 2022.
This umbrella review included 57 meta-analyses involving 19 unique outcomes of the correlation between vitamin C intake and cancers.
4.4. History and controversy of vitamin C use in cancer
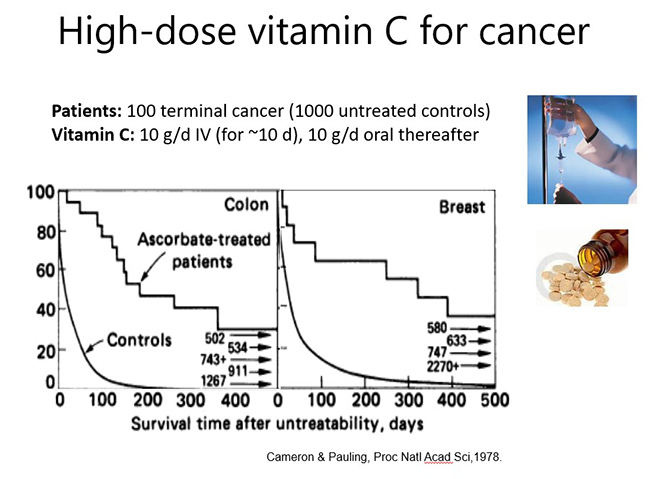
The use of vitamin C for the prevention and treatment of cancer is fraught with controversy. However, much of the controversy around vitamin C use in cancer therapy has arisen from early misunderstandings around the pharmacokinetics of oral versus intravenous vitamin C. In the mid-1970s Cameron and Pauling published findings from 100 terminal cancer patients who had been administered 10 g/day IV vitamin C for approximately 10 days, followed by 10 g/day oral vitamin C thereafter. Their work showed significantly enhanced survival in these patients compared with two retrospective cohorts of 1,000 patients who did not receive vitamin C (see figure below).
Subsequently, researchers at the Mayo Clinic attempted to reproduce these findings with two RCTs carried out in 123 patients with advanced malignancies and 100 patients with advanced colorectal cancer (see figure below). Neither study showed a significant survival advantage in the patients who received vitamin C. The negative results of the Mayo Clinic RCTs relegated the use of vitamin C to the arena of complementary and alternative medicine.
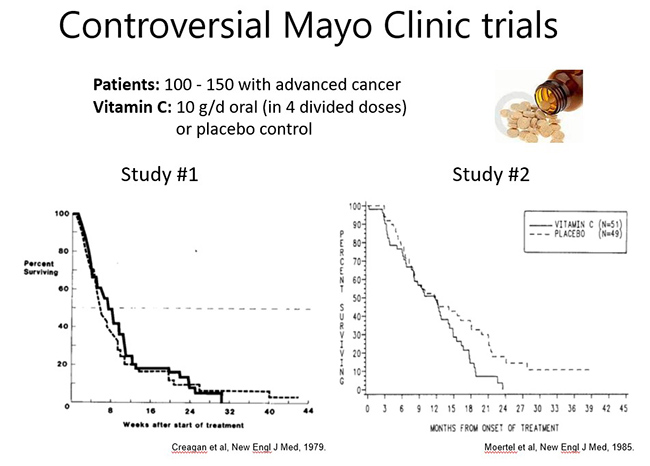
It wasn't until the mid-1990s, when the seminal work by Mark Levine's group highlighted the dramatic differences between the pharmacokinetics of oral and IV vitamin C (covered in Module 1), that the discrepancies between the original Cameron and Pauling studies and the Mayo Clinic RCTs were explained. While Cameron and Pauling had used IV vitamin C with subsequent oral maintenance, the Mayo Clinic RCTs comprised divided daily doses of oral vitamin C only. The realisation that IV vitamin C may be more effective than oral vitamin C in oncology patients sparked a surge of new research in the field over the subsequent years.
4.5. Vitamin C mechanisms of action in cancer
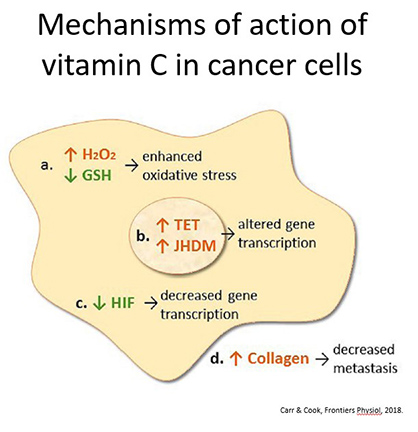 A number of mechanisms of action for vitamin C in cancer have been proposed (see figure below). These include: enhancing oxidative stress through a 'pro-oxidant' mechanism, down-regulating gene transcription of pro-survival factors, epigenetic regulation, collagen-dependent inhibition of metastasis, and the ability of high doses to penetrate into the core of solid tumours.
A number of mechanisms of action for vitamin C in cancer have been proposed (see figure below). These include: enhancing oxidative stress through a 'pro-oxidant' mechanism, down-regulating gene transcription of pro-survival factors, epigenetic regulation, collagen-dependent inhibition of metastasis, and the ability of high doses to penetrate into the core of solid tumours.
Currently, one of the most widely accepted anti-cancer mechanisms proposed for high-dose vitamin C is based on its so-called 'prooxidant' activity. However, this terminology can be misleading as vitamin C itself always acts as an antioxidant, through donation of electrons; the 'pro-oxidant' action occurs subsequently and is therefore an indirect effect. As such, the term 'pro-drug' has been adopted by some researchers.
In vitro, vitamin C (in the form of the ascorbate anion) is able to reduce transition metal ions, such as iron III (Fe3+) and copper II (Cu2+) cations (reaction I). The reduced transition metal ions are then able to generate hydrogen peroxide (H2O2) through reduction of oxygen to the superoxide radical (reaction II), which can also react with itself to form hydrogen peroxide (reaction III).
I. AH- + Fe3+/Cu2+ → A•- + Fe2+/Cu+ + H+
II. Fe2+/Cu+ + O2 → Fe3+/Cu2+ + O2•- + H+
III. 2O2•- + 2H+ → H2O2 + O2
However, whether catalytically available transition metal ions are found in vivo and can cause enhanced oxidative stress is still a matter of some debate since iron and copper are normally sequestered in transport and storage proteins such as transferrin, ferritin and ceruloplasmin. During tissue injury, transition metal ions may become more catalytically available. It has also been postulated that transition metal ions are catalytically more available in the extracellular fluid of the tumour microenvironment.
Pharmacokinetic studies in oncology patients have provided insight into the doses of IV vitamin C required to generate high (millimolar) concentrations of vitamin C in plasma; it is generally believed that plasma vitamin C concentrations >20 mmol/L are required for hydrogen peroxide generation in vivo.
Although H2O2 has not been detected in whole blood following vitamin C infusion, our research has shown that erythrocytes (RBCs) accumulate low millimolar concentrations of vitamin C during IV vitamin C infusions which stimulates autoxidation of iron within haemoglobin and generation of H2O2 inside the cells (through the above reaction pathways). This is an issue for people with G6PD deficiency, as you learnt in Module 1, due to an inability to neutralise the generated H2O2.
Administration of high dose parenteral vitamin C (i.e., 1–8 g/kg/day) to murine models has been shown to decrease tumour growth and enhance survival. The 'pro-oxidant' activity of vitamin C is thought to predominate at these higher doses. However, it should be noted that the doses of vitamin C administered to animal models are typically four to eight times higher and more frequent (daily vs. twice a week) than those administered to patients. As yet, there is little evidence to indicate that the 'pro-oxidant' mechanism is occurring in oncology patients administered IV vitaminC (other than inside RBCs).
Further reading:
-
The unpaved journey of vitamin C in cancer treatment. Chen et al. Can J Physiol Pharmacol, 2015.
This review, by one of the pioneering researches in the field, describes the research behind the 'pro-oxidant' mechanism of vitamin C and the downstream cellular effects.
4.5.1. Gene transcription
Animal studies, particularly in vitamin C-requiring animals such as Gulo knockout mice and guinea pigs, have indicated that oral dosing (e.g., 0.3–5 g/L) and low parenteral doses of vitamin C (e.g., 0.1 g/kg/day) exhibit comparable decreases in tumour growth to high dose parenteral vitamin C (i.e., 1–8 g/kg/day). Since hydrogen peroxide is not detected following oral or low dose IV vitamin C administration, this suggests possible tumour growth inhibition mechanisms other than hydrogen peroxide generation are likely operating in these situations.
Preclinical studies have shown regulatory effects of vitamin C administration on various transcription factors and cell signalling pathways, with subsequent effects on cell cycle, angiogenesis, and cell death pathways. Analysis of tissues from various animal models has indicated regulation of numerous genes and their products following administration of vitamin C. Thus, it appears that vitamin C administration, particularly at lower doses, has gene-regulatory effects.
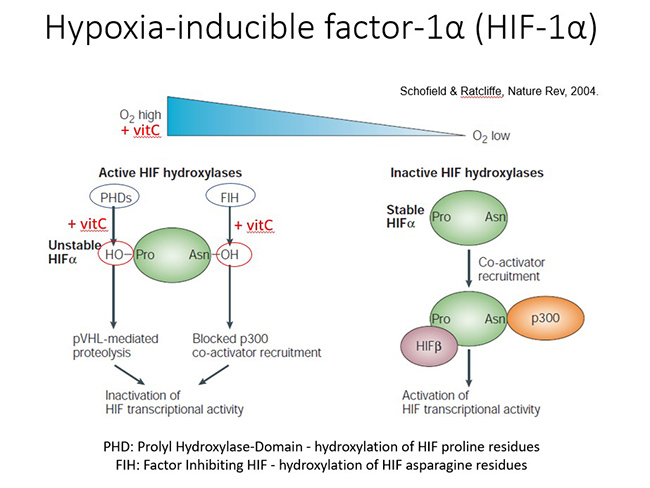
In the early 2000s, vitamin C was demonstrated to regulate the transcription factor hypoxia inducible factor-1α (HIF-1 α; see figure below). HIF-1α regulates numerous genes driving tumour survival, angiogenesis, stem cell phenotype and metastasis. HIF is upregulated in the hypoxic core of solid tumours due to the absence of substrates and cofactors, such as vitamin C, which is required for hydroxylase-dependent downregulation of HIF-1α.
Animal studies have shown downregulation of HIF-1α and downstream pro-survival proteins following administration of oral or parenteral vitamin C. In human colorectal tumours and other tumours there was an inverse association between tumour vitamin C levels and expression of HIF and related downstream proteins, and enhanced disease-free survival was observed in patients who had higher vitamin C levels in their tumours.
Further reading:
-
Ascorbate as a co-factor for fe- and 2-oxoglutarate dependent dioxygenases: physiological activity in tumor growth and progression. Kuiper and Vissers. Front Oncol, 2014.
This review highlights research around regulation of gene transcription by vitamin C in cancer.
4.5.2. Epigenetic modification
Recent research has uncovered a role for vitamin C in epigenetic regulation via acting as a cofactor for DNA and histone hydroxylases which belong to the same family of enzymes as collagen and HIF hydroxylases. Vitamin C acts as a cofactor for the ten-eleven translocation (TET) dioxygenases which hydroxylate methylated cytosine moieties in DNA (see figure below). The hydroxymethylcytosine moiety may represent an epigenetic mark in its own right, and it can be further oxidized and subsequently removed through both active and passive DNA repair mechanisms, resulting in demethylation with subsequent effects on DNA transcription. It is noteworthy that a decrease in DNA hydroxymethylation has been observed in cancer cells and tumors.
Research has indicated that vitamin C can modulate the epigenome of leukaemia cells and regulate hematopoietic stem cell function in a TET-dependent fashion, suppressing leukemia progression in pre-clinical models. Research has also indicated that vitamin C treatment increases hydroxymethylation in lymphoma and melanoma cells, and causes a decrease in tumour-cell invasiveness and clonogenic growth. Thus, epigenetic mechanisms may be involved in the attenuated metastasis that has been observed in animal models and patients following administration of vitamin C.
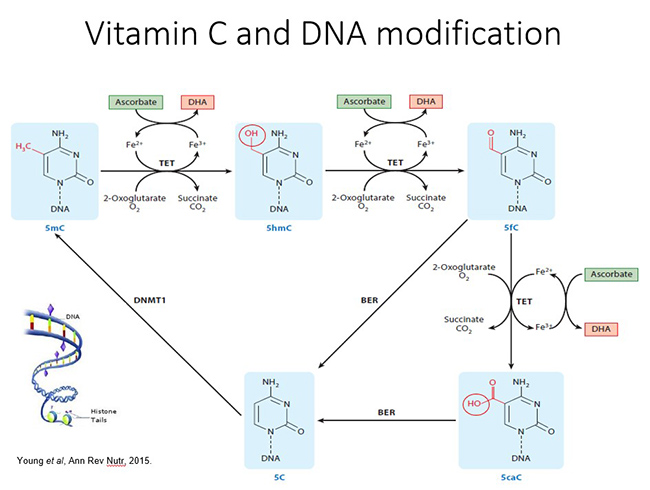
Vitamin C is also a cofactor for several Jumonji C domain-containing histone demethylases (JHDM) that catalyze histone demethylation (see figure below). Methylation of lysine and arginine residues on histones is closely associated with activation or silencing of transcription. Vitamin C is required for optimal catalytic activity and demethylation by JHDM. The involvement of vitamin C in JHDM-dependent histone demethylation was confirmed in somatic cell reprogramming and T-cell maturation.
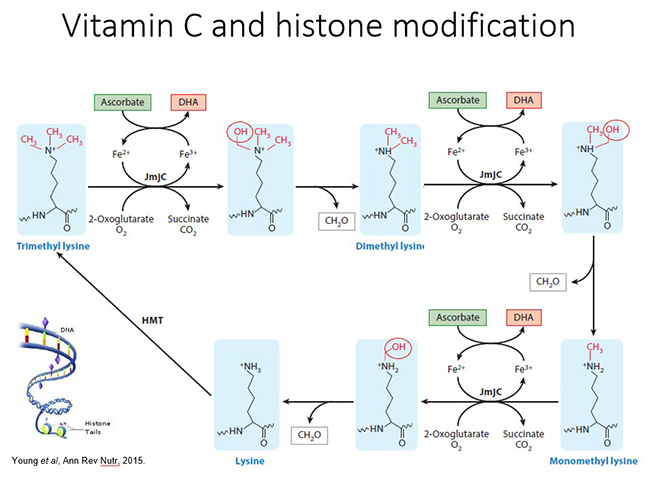
Thus, it appears that vitamin C can regulate the epigenome via acting as a cofactor for both DNA and histone demethylases. Of note, oral dosing of vitamin C (500 mg/day) was shown to be sufficient to normalise vitamin C concentrations and induce epigenetic changes in patients undergoing treatment for myeloid cancer. Due to the multitude of genes regulated through both DNA and histone demethylation, it is likely that epigenomic regulation by vitamin C may play a major role in its pleiotropic health promoting and disease modifying effects.
Further reading:
-
The role of vitamin C in epigenetic cancer therapy. Mikkelsen et al. Free Radic Biol Med, 2021.
This review highlights the research around epigenetic regulation by vitamin C in cancer.
4.5.3. Collagen synthesis and metastasis
Vitamin C has long been known to be a cofactor for the hydroxylase enzymes essential for the stabilization of collagen tertiary structure. Research has shown increased collagen encapsulation of tumours in Gulo knockout mice with melanoma and breast tumours following supplementation with low dose oral vitamin C (0.15 g/L). Decreased metastases were also observed in these models.
This work has been confirmed in a pancreatic cancer model; increased levels of collagen were detected in tumour stroma of vitamin C-treated mice and this was associated with decreased tumour invasion. Resected tumours from pancreatic cancer patients treated with IV vitamin C also exhibited increased collagen content (see further reading below). Since enhanced collagen mRNA levels were also observed in the tumors from vitamin C-treated mice, this suggests that gene regulatory mechanisms are also involved.
Further reading:
-
High dose parenteral ascorbate inhibited pancreatic cancer growth and metastasis: Mechanisms and a Phase I/IIa study. Polireddy et al. Sci Rep. 2017.
This paper comprises preclinical research and a small Phase I/IIa study (n = 14) which investigated the mechanisms involved in inhibition of pancreatic cancer growth and metastasis.
4.5.4. Penetration into solid tumours
Studies investigating the vitamin C content of tumour tissue removed from patients with colorectal cancer showed lower vitamin C concentrations in the tumour tissue relative to matched normal tissue. Furthermore, higher grade colorectal, endometrial and breast tumors had proportionately less vitamin C than lower grade tumors. Of note, higher tumour vitamin C content was associated with increased disease-free survival (see figures below).
In vitro research has indicated that vitamin C has poor penetration into tumour tissues as these are generally poorly vascularised which impairs nutrient delivery. However, higher, pharmacological concentrations of vitamin C are able to penetrate into tumour tissue. The investigators demonstrated that supra-physiological plasma concentrations (i.e., up to 500 µmol/L) were required to achieve effective delivery of vitamin C to poorly vascularized tumour tissue.
A small clinical study has indicated that high-dose intravenous vitamin administration to patients with colon cancer (1 g/kg/day for four days) resulted in increased vitamin C content of their tumour tissue (see further reading below). Enhanced delivery of vitamin C to the hypoxic core of solid tumors would conceivably facilitate regulation of HIF-1α and epigenetic pathways within the hypoxic core of the tumour. The generally better efficacy of IV vitamin C against metastatic tumors could be due, in part, to the generally smaller size of metastases allowing better diffusion of vitamin C into the tumour, thus facilitating its various gene-regulatory mechanisms.
Further reading:
-
Vitamin C administration by intravenous infusion increases tumor ascorbate content in patients with colon cancer: A clinical intervention study. Dachs et al. Front Oncol, 2021.
This research study reported an increase in the vitamin C content of colorectal tumours after IV vitamin C administration to patients.
4.5.5. Antioxidant and anti-inflammatory activities
It has been suggested that oxidative stress, chronic inflammation, and cancer are closely linked. As you learnt in Module 1, vitamin C is a potent antioxidant both in plasma and within cells due to its ability to scavenge a wide range of reactive oxygen species, thereby protecting important biomolecules from oxidative damage. Patients with cancer tend to have elevated markers of oxidative stress. Administration of high dose IV vitamin C to patients with pancreatic cancer produced a decrease in F2-isoprostanes, a marker of systemic oxidative stress, suggesting a systemic antioxidant effect of IV vitamin C.
Oxidative stress can activate a variety of transcription factors, leading to the expression of hundreds of different genes, including those of proinflammatory cytokines. Elevated markers of inflammation (such as C-reactive protein and various cytokines), have been reported in oncology patients. Vitamin C exhibits anti-inflammatory functions via modulating cytokine levels and in patients with various cancers, administration of 25–50 g IV vitamin C decreased a number of different inflammatory mediators (such as C-reactive protein) and pro-inflammatory cytokines.
Because oxidants can enhance inflammation, it is not clear if the cytokine-modulatory effects of vitamin C are due to its oxidant scavenging function or its gene regulatory cofactor functions. It is noteworthy that patients with higher levels of inflammation also appear to have a higher requirement for vitamin C.
4.5.6. Optional activity: cancer podcast
Timing: approx. 80 min.
Listen to this podcast on 'Vitamin C for Cancer Treatment' by Prof Margreet Vissers.
Further reading:
-
Potential mechanisms of action for vitamin C in cancer: Reviewing the evidence. Vissers and Das. Front Physiol. 2018.
This review covers the proposed mechanisms of vitamin C in cancer, primarily the 'pro-oxidant mechanism, and the vitamin C-dependent enzymes that regulate gene transcription and epigenetics.
4.6. Does vitamin C interfere with chemotherapy or radiotherapy?
4.6.1. Vitamin C and chemotherapy
Potential interactions between vitamin C and chemotherapeutic agents have long been a matter of debate. Because of vitamin C's potent antioxidant activity, many clinicians believe they have to avoid the concurrent use of IV vitamin C during all chemotherapy regimens. However, different chemotherapeutic agents act via different mechanisms, and only some act via oxidative mechanisms.
Nevertheless, it has been recommended for administered natural therapies to allow five half-lives to elapse prior to administration of chemotherapeutic agents to eliminate potential interactions. Because vitamin C has a relatively short half-life of <2 h in circulation due to rapid renal clearance, IV vitamin C is typically administered the day before or after chemotherapy administration. However, if the chemotherapeutic agent does not act via oxidative mechanisms, then concurrent IV vitamin C administration may not be an issue and would be more patient centred.
Animal studies have indicated that concurrent administration of vitamin C with numerous different chemotherapeutic agents (e.g., gemcitabine, paclitaxel, carboplatin, melphalan, carfilzomib, bortezomib, cisplatin, and temozolomide) synergistically decreased xenograft tumour growth, including in a chemotherapy resistant pancreatic tumour model, and synergistically increased survival. The antitumor activity of some (e.g. dacarbazine and valproic acid) was not affected when combined with high dose parenteral vitamin C and administration of vitamin C reduced the toxic side effects of others (e.g. paclitaxel and doxorubicin) without interfering with their antitumor effects. Interestingly, many of the pre-clinical studies showed that administration of IV vitamin C alone was as effective at decreasing tumour growth and promoting survival as the chemotherapeutic agents themselves.
Human trials have shown no adverse effects from combining IV vitamin C with a number of different chemotherapeutic agents (e.g., carboplatin, paclitaxel, decitabine, cytarabine, aclarubicin, gemcitabine, erlotinib, and temozolomide), and in many cases decreased off-target toxicity and improved health-related quality of life were observed. Vitamin C is routinely administered in combination with arsenic trioxide to enhance its efficacy in the treatment of refractory multiple myeloma.
4.6.2. Vitamin C and radiotherapy
Radiotherapy with ionizing radiation generates free radicals and also increases levels of catalytic transition metal ions in tissues. A few studies have been carried out in animal models, with most showing radio-sensitising effects of high dose vitamin C in combination with ionising irradiation. High dose vitamin C administration was shown to act synergistically with radiotherapy, decreasing tumour growth and enhancing survival.
One study showed radioprotective effects of high dose vitamin C. These differences likely reflect the timing of the radiation treatment relative to vitamin C administration. For example, in the latter study, radiation treatment was carried out only 2 h after intraperitoneal administration of vitamin C, while in the other studies radiation treatment was carried out on days 3 or 5 following initiation of high dose vitamin C administration.
PET imaging showed tumouristatic activity of vitamin C administration alone and radiation therapy alone, however, the two combined showed tumouricidal activity. More studies need to be carried out to determine appropriate tumour models and optimal timing and dosing of IV vitamin C combined with radiotherapy.
4.6.3. Vitamin C and chemotherapy-related toxicity
Numerous animal studies have shown decreased off-target toxicity of chemotherapeutic agents following administration of oral and IV vitamin C. For example, vitamin C administration decreased white blood cell loss, weight loss, ascites accumulation, hepatotoxicity, reticulocytosis, lipid oxidation, and cardiomyopathy induced by the chemotherapeutic agents (e.g. carboplatin, paclitaxel, doxorubicin and cisplatin, the latter of which is known to cause off-target oxidative stress).
Furthermore, it has been noted that combination therapy with vitamin C synergistically enhances sensitivity to specific anti-cancer drugs, thus potentially decreasing the required dosage and ameliorating associated side-effects. Low dose IV vitamin C (e.g., 1 g/infusion) is often administered with arsenic trioxide for multiple myeloma or leukaemia to improve tolerability of the chemotherapeutic agent.
Decreased chemotherapy-related toxicity has been demonstrated in patients with stage III–IV ovarian cancer receiving chemotherapy (carboplatin and paclitaxel) in conjunction with high-dose IV vitamin C (75–100 g two times per week) (see further reading below). Adverse events were evaluated and grade 1 and 2 toxicities were found to be significantly decreased in the group receiving IV vitamin C. Decreased toxicities were observed in almost all the evaluated organ systems. Of note, despite decreasing chemotherapy-related toxicity, IV vitamin C did not appear to adversely affect the anti-cancer activity of the drugs as assessed by survival of the patients or time to disease relapse or progression.
In support of a role for vitamin C in decreasing chemotherapy-related toxicity, a Phase I clinical study of patients with pancreatic cancer treated with gemcitabine reported decreased plasma F2-isoprostanes, an established oxidative stress biomarker, following administration of high dose IV vitamin C. Thus, IV vitamin C is a potentially useful adjunctive therapy to decrease off-target toxicity of chemotherapeutic agents and as a result may also improve the health-related quality of life of oncology patients.
Further reading:
-
High-dose parenteral ascorbate enhanced chemosensitivity of ovarian cancer and reduced toxicity of chemotherapy. Ma et al. Sci Transl Med, 2014.
This translational research showed that the combination of IV vitamin C with the chemotherapeutic agents carboplatin and paclitaxel synergistically inhibited ovarian cancer in a mouse model and reduced chemotherapy-associated toxicity in patients with ovarian cancer.
4.7. Vitamin C and cancer-related quality of life
Patients with cancer commonly experience a number of symptoms of disease progression and the side-effects of radiation therapy and adjuvant chemotherapy that adversely impact on their quality of life. Since the early 1970s and 1980s, clinicians have reported improved subjective quality of life in patients following administration of both high dose oral and IV vitamin C. More recent studies specifically assessing the effects of IV vitamin C administration on cancer- and chemotherapy-related quality of life using validated questionnaires have shown decreases in common symptoms, such as fatigue, pain, nausea/vomiting, insomnia and appetite loss, following administration of IV vitamin C (see figure below).
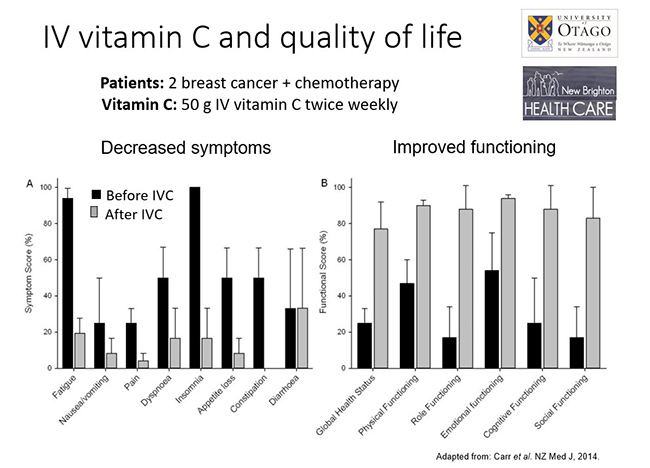
These studies also demonstrated improvements in overall health and, specifically, enhanced physical, emotional, cognitive, and social functioning. Interestingly, even relatively low IV vitamin C doses of 2.5–10 g/infusion provided decreased symptoms and improved quality of life, suggesting that antioxidant/anti-inflammatory functions and/or enzyme cofactor mechanisms of vitamin C may be involved in the quality of life improvements.
Further reading
-
The effect of intravenous vitamin C on cancer- and chemotherapy-related fatigue and quality of life. Carr et al. Front Oncol, 2014.
This review discusses the evidence behind vitamin C's quality of life effects in patients with cancer, with and without chemotherapy.
4.8. Intravenous vitamin C use in clinical practice
Since publication of the negative Mayo clinic RCTs, few vitamin C and cancer RCTs have been carried out. There has been significant inconsistency in the doses, frequency and duration of therapy and types of cancer investigated. Many of the earlier studies recruited terminal or end-stage patients, for whom any sort of treatment is unlikely to have an effect, and they often recruited cohorts with mixed cancers, which may respond differentially to IV vitamin C depending on the underlying mechanisms involved. The table below shows examples of small/pilot RCTs and clinically-relevant outcomes.
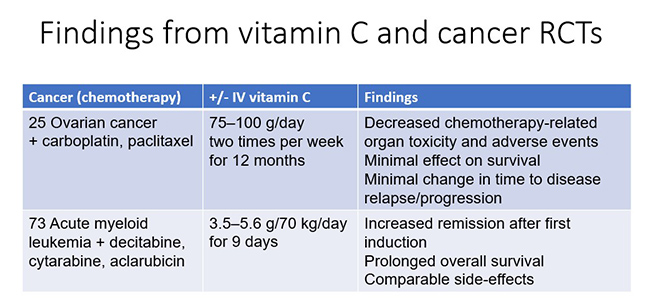
It is unlikely that future large-scale IV vitamin C RCTs will be carried out due to the prohibitive costs. Nevertheless, smaller scale studies, if well designed, have the potential to contribute relevant and translatable findings to inform good clinical practice. For example, future work should focus on tailoring IV vitamin C regimens to specific cancers or cancer subtypes, e.g., haematological cancers that are driven specifically by TET mutations may respond more readily to IV vitamin C therapy.
4.8.1. Activity: cancer audiovisual
Timing: approx. 30 min.
Watch this presentation by Dr Jeanne Drisko on “Ovarian and pancreatic cancer trials” (from the Vitamin C Symposium: from bench to bedside).
4.8.2. Safety of IV vitamin C
IV vitamin C is remarkably safe, considering the massive (≥75 g) doses that are often administered. However, there are several currently known situations where caution is warranted (these have been covered in more detail in Module 1). These include patients with impaired renal function due to their inability to adequately clear high IV vitamin C doses from circulation, and patients with G6PD deficiency due to inability to detoxify oxidative stress generated within their RBCs. Caution is also required for patients requiring regular glucose monitoring due to the potential for IV vitamin C to interfere with point-of-care glucose monitors.
High dose intravenous vitamin C has been administered by physicians for many decades as a complementary and alternative therapy for oncology patients, with a very high safety profile (see further reading below). Of 9,328 patients surveyed, only 1% reported minor side effects that included lethargy, fatigue, change in mental status and vein irritation. More recent Phase I safety trials of high dose IV vitamin C indicate only minor side effects and no adverse events over and above what would be expected from the underlying disease or chemotherapy side effects (keeping in mind the specific contraindications discussed above).
4.8.3. What are the optimal doses?
A survey of complementary and alternative medicine practitioners showed an average dose of 28 g/infusion (range of 1–200 g/infusion) (see further reading below). Because of the prevailing 'pro-oxidant' paradigm of IV vitamin C, it is generally believed that 'more is better' and doses as high as 200 g/infusion have been administered to oncology patients. Lower IV vitamin C doses of 2.5–10 g/infusion have been shown to decrease common cancer- and chemotherapy-related symptoms and improve health-related quality of life.
Although the 'pro-oxidant' activity of IV vitamin C has yet to be conclusively demonstrated in humans, there may be alternate rationales for administering high dose IV vitamin C. Solid tumours exhibit dysregulated blood supply which limits diffusion of oxygen and other nutrients to the core of the tumours. The minimum vitamin C doses required for diffusion into solid tumours are not yet known.
Oral vitamin C doses (500 mg/day) have been shown to regulate epigenetic profiles in patients undergoing treatment for myeloid cancer, although the potential health benefits of this are not yet known. Uptake of vitamin C (particularly low doses) into tumour cells may be dependent upon vitamin C transporter (SVCT2) status and associated polymorphisms.
4.8.4. What is the optimal frequency?
A survey of complementary and alternative medicine practitioners showed an average frequency of IV vitamin C infusions of approximately twice a week (range of 1–7 times per week) (see further reading below). Preclinical studies indicate that a single infusion of vitamin C is not as effective as multiple infusions and a higher frequency of administration appears to be more beneficial. For example, daily intraperitoneal injections of vitamin C slowed tumour growth in the mice and downregulated HIF-1α and downstream gene products to a greater extent than injections every other day. Daily administration of high dose IV vitamin C to rodents with implanted prostate tumour cells showed decreased tumor growth and lung metastases. In contrast, a trial of patients with castration-resistant prostate cancer who were administered only one 60 g infusion per week did not show diminished PSA levels or disease remission after 12 weeks.
Although continuous vitamin C infusion has been piloted, this is usually only practical if the patients are hospitalised. However, because IV vitamin C solutions are remarkably stable, even at ambient temperature and in the light, it might be possible to utilize continuous infusion bottles typically used for home intravenous antibiotic administration. However, since intermittent infusions allow for high peak plasma concentrations, there is debate as to whether continuous infusion is better than intermittent infusions over a longer period. As mentioned earlier, high peak concentrations may be required to facilitate uptake of vitamin C into solid tumours.
4.8.5. What is the optimal duration?
A survey of complementary and alternative medicine practitioners showed an average duration of about 19 treatments per patient (range of 1–80 treatments) (see further reading below). The optimal duration will be highly individual and will depend on many factors e.g. type of cancer, stage and, depending on the underlying mechanisms involved, it is possible that antitumor activity may require long term treatment and follow-up, e.g., over years rather than the few weeks or months of most clinical trials.
Further reading:
-
Vitamin C: intravenous use by complementary and alternative medicine practitioners and adverse effects. Padayatty et al. PLoS One, 2010.
This survey of users of IV vitamin C highlighted the indications and contraindications for IV vitamin C use in clinical practice. -
Intravenous ascorbic acid protocol for cancer patients: scientific rationale, pharmacology, and clinical experience. Mikirova et al. Functional Foods in Health and Disease, 2013.
The Riordan Clinic in Kansas, USA, has been administering IV vitamin C to patients for many decades and presents their protocol as an appendix in this publication.
Additional resources:
- See Module 6 for information on IV vitamin C administration for practitioners.
4.9. Summary of Module 4
- People with cancer typically have lower vitamin C concentrations than healthy controls, and these tend to be even lower with higher burden or higher stage disease. Administration of chemotherapeutic drugs can further deplete vitamin C levels.
- Meta-analyses of epidemiological studies have consistently shown associations between increased vitamin C intake and plasma concentrations and decreased risk of cancer, including gastric, breast, cervical, prostate, lung, oesophageal, pancreatic, renal, and brain cancer (glioma).
- Early vitamin C and cancer trials used intravenous vitamin C followed by oral vitamin C, whereas subsequent (Mayo Clinic) RCTs used oral vitamin C only. These latter trials did not show any survival advantage, in contrast to the earlier studies. The discrepancy in findings is likely due to the very different pharmacokinetics of oral versus intravenous vitamin C.
- Vitamin C has a number of proposed mechanisms of action in cancer. These include: enhancing oxidative stress through a 'pro-drug' mechanism, down-regulating gene transcription of pro-survival factors, epigenetic regulation, and collagen-dependent inhibition of metastasis. There is also evidence for anti-inflammatory and antioxidant mechanisms in oncology patients. Pharmacologic doses may be required to aid in penetration of the vitamin into solid tumours.
- Vitamin C does not interfere with most chemotherapeutic agents, but can potentially interfere with radiotherapy so doses and timing of administration are more critical. Vitamin C decreases off-target chemotherapy-related toxicity and attenuates common symptoms, such as fatigue, pain, nausea/vomiting, insomnia and appetite loss, thus improving patient quality of life.
- High-dose intravenous vitamin C has been administered for many decades and Phase I trials indicate a relatively good safety profile. However, few RCTs have been carried out so clinically relevant information such as optimal doses, frequency and durations are not yet certain and will likely vary depending on the type of cancer, stage and underlying mechanisms involved.
4.10. Activity: Self-reflection and feedback
Once you have completed all the Modules of interest to you, please complete the self-reflection and feedback form online or email to anitra.carr@otago.ac.nz. For members of the RNZCGP, please include your MCNZ number and the modules completed so that your CPD credits can be uploaded to the RNZCGP website. A certificate of completion can be emailed to you if required.
- Self-reflection and feedback form (online)
- Self-reflection and feedback form (DOCX)
© Anitra Carr, 2022. You may not copy, modify, distribute, display, transmit, perform, publish or sell any of the copyrightable material on this website. You may hyperlink to this website but must include the following statement: "This link leads to the website 'Oral and intravenous vitamin C use in health care' provided by the Nutrition in Medicine Research Group at University of Otago, Christchurch."
