 There are a variety of different ways to find out if someone is infected with the coronavirus SARS-CoV-2, which causes the disease called Covid-19. The most accurate is called a PCR test.
There are a variety of different ways to find out if someone is infected with the coronavirus SARS-CoV-2, which causes the disease called Covid-19. The most accurate is called a PCR test.
The PCR test looks for the genetic material of the virus in a swab sample taken from a person's nose or throat. It involves making lots of copies of a piece of the virus's genetic material so we can see if it is there or not.
PCR is also one of the most important techniques that we use in our research at the Otago Department of Biochemistry.
But how does it actually work?
1) Take a swab
What is happening with those long sticks up people's noses?

A healthcare worker about to swab someone for a coronavirus test.
To find out if a person has coronavirus, a healthcare worker uses a swab with a long shaft to gently scrape the back of the nasopharynx of that person. The nasopharynx is the upper part of the throat, right behind behind the nose. Not very comfortable!
This is where your nasopharynx is:
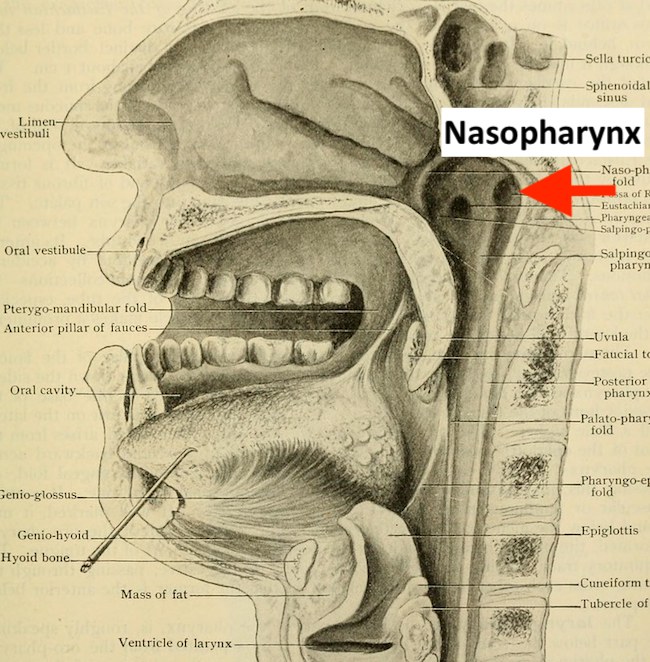
Image from "Human anatomy, including structure and development and practical considerations" (1911) on www.flickr.com
After scraping the nasopharynx, the end of the swab will have some of the person's cells and mucus on it, as well as any bacteria or viruses that were sitting back there.
The swab is quickly put into a tube containing a mix of protein and antibiotics that keeps any collected virus safe, then the tube is sealed and sent to a testing laboratory.
You can see how a swab is taken in this video made by the medical education company AMBOSS.
Problems with swabbing
Usually, if someone is infected with the virus and is showing symptoms, the swab should be able to pick up virus particles from the nasopharynx.
However, sometimes the virus might be multiplying in places away from where the swab is, or there is not yet enough virus around for the swab to pick up.
So a negative test might mean that you don't have coronavirus, or that you have coronavirus and it just isn't detectable yet, or the wrong part was swabbed.
Then send the swab sample to a laboratory
Hopefully the courier is fast!
2) Get the RNA genetic material out and clean it up
What we're dealing with:
The coronavirus is made up of two main parts: an oily membrane around the outside, studded with proteins that stick out of the surface, and genetic material called RNA on the inside, with more proteins tightly wrapped around it.
Here is a drawing of a coronavirus particle cut in half so you can see the inside. The proteins sticking out of the outside membrane are drawn in pink. Inside you can see the thin, squiggly RNA wrapped up in purple proteins.

Illustration by David S. Goodsell, RCSB Protein Data Bank.
To do the test to check for coronavirus, we have to break open the virus particles to get out the genetic material. We also need to get rid of everything else in the sample that could stop the test from working.
The swab sample will have lots of stuff in it, including mucus and human cells as well as viruses. The human cells are also made up of proteins, membrane, DNA, and RNA.
That means we will need to get rid of the parts of the virus that we don't need for the test (proteins and oily membrane) and everything else in the sample – the proteins, oily membranes and DNA from the mucus and human cells.
So… break up the molecules we don't want...
We break open the virus particles using some chemicals – a detergent and something called a chaotropic salt.
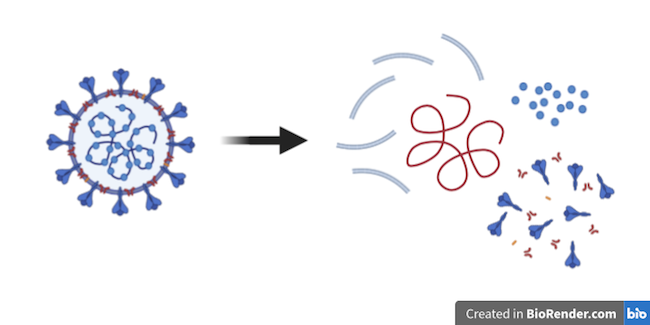
Breaking the virus into bits releases its RNA (the squiggly line in red).
The detergent helps to break open the membranes of cells and viruses, which are both made up of oily molecules.
The chaotropic salt has several roles. It denatures, or unravels, the many different proteins in the sample, stopping them from working, and helps separate the RNA from any proteins wrapped around it.
We chop up the proteins in the sample into bits using an enzyme called a protease, and we chop up the DNA in the sample into bits using an enzyme called a DNase.

…Then get rid of everything except the RNA.
Now we have a tube with lots of different types of broken-up molecules in it, mixed in with RNA. We need to get rid of everything except the RNA.
To make sure we keep the RNA and not wash it away accidentally, we add little silica (glass) magnetic beads. The RNA sticks to the silica beads, helped by the chaotropic salts. Then we put a magnet on the outside of the tube. The beads (and therefore the RNA) stick to the inner wall of the tube, held there by the magnet on the outside.
With the magnet holding the beads and RNA in place, you can easily wash all the remaining bits of unwanted molecules away without losing the RNA. Adding liquid with some more chaotropic salt will help to do this, then we can wash the salt away using some alcohol.
Once the RNA is clean, we can unstick it from the magnetic silica beads simply by washing the beads with water. When the RNA is in the water, and not on the beads anymore, we can get rid of the beads using the magnet again.
This gif shows you the steps we use to clean up the RNA:
3) Make sure the test will only detect the new coronavirus
The PCR test is so precise that it can tell the difference between the seven coronaviruses that are known to cause diseases in humans.
| This virus: | causes this disease: |
|---|---|
| SARS-CoV | SARS |
| SARS-CoV-2 | Covid-19 |
| MERS-CoV | MERS |
| HCoV-OC43 | Common cold |
| HCoV-HKU1 | Common cold |
| HCoV-229E | Common cold |
| HCoV-NL63 | Common cold |
The RNA left in your sample will be a mixture of human RNA and RNA from any bacteria or viruses in the nasopharynx of the person who was swabbed.
To make sure we only detect the coronavirus RNA, and not the DNA or RNA of any other organism, we need to find a little bit of the coronavirus RNA sequence that is unique to the coronavirus, and is not shared by any other living thing.
The RNA of the new coronavirus was sequenced by scientists early in the outbreak. There are nearly 30,000 bases (letters) in the coronavirus genome, containing the instructions for making 29 different proteins.
Here is a diagram of that genome:
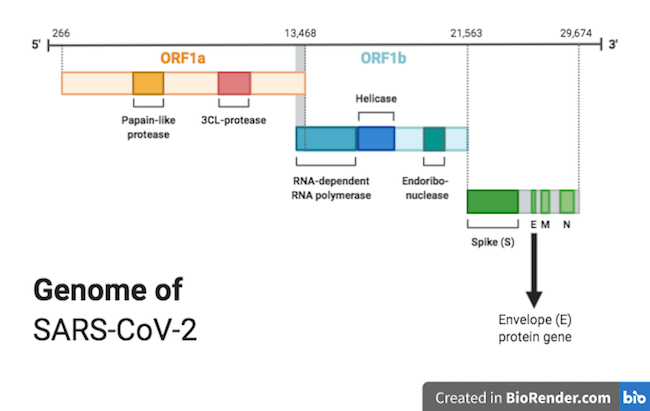
We need to make two short pieces of DNA ('primers') that will only stick to somewhere on that genome sequence.
Scientists chose two short pieces of the sequence in gene E, 22 and 26 bases long, for the PCR test. The E (envelope) protein encoded by this gene helps to form the oily membrane of the virus.
The scientists made DNA primers that only stick to those pieces of gene E and nowhere else.
(By the way, DNA and RNA do stick together, if they have the right sequences.)
Here is the RNA sequence of the E gene (RNA is made up of G, C, A and U bases):
AUGUACUCAUUCGUUUCGGAAGAGACAGGUACGUUAAUAGUUAAUAGCGUACUUCUUUUUCUUGCUUUCGUGGUAUUCUU
GCUAGUUACACUAGCCAUCCUUACUGCGCUUCGAUUGUGUGCGUACUGCUGCAAUAUUGUUAACGUGAGUCUUGUAAAAC
CUUCUUUUUACGUUUACUCUCGUGUUAAAAAUCUGAAUUCUUCUAGAGUUCCUGAUCUUCUGGUCUAAACGAACUAAAUA
UUAUAUUAGUUUUUCUGUUUGGAACUUUAAUUUUAGCC
And here are the sequences of the two DNA primers used in the test (DNA is made up of G, C, A and T bases):
Forward primer: ACAGGTACGTTAATAGTTAATAGCGT
Reverse primer: ATATTGCAGCAGTACGCACACA
The primers will only stick to the E gene on the parts underlined here:
AUGUACUCAUUCGUUUCGGAAGAGACAGGUACGUUAAUAGUUAAUAGCGUACUUCUUUUUCUUGCUUUCGUGGUAUUCUU
GCUAGUUACACUAGCCAUCCUUACUGCGCUUCGAUUGUGUGCGUACUGCUGCAAUAUUGUUAACGUGAGUCUUGUAAAAC
CUUCUUUUUACGUUUACUCUCGUGUUAAAAAUCUGAAUUCUUCUAGAGUUCCUGAUCUUCUGGUCUAAACGAACUAAAUA
UUAUAUUAGUUUUUCUGUUUGGAACUUUAAUUUUAGCC
This is how the test will only detect the RNA of coronavirus, and not the RNA of anything else.
4) If the virus is there, make DNA!
Time for some RT-PCR
To detect any coronavirus RNA present, we need to make lots and lots of copies of it, but we can't easily make lots of copies of RNA directly.
Therefore, we first have to make a DNA copy of the RNA. This is called reverse transcription (RT), which we do using an enzyme called reverse transcriptase.
Once we have the DNA copy, then we can make loads of copies of that using the polymerase chain reaction (PCR) and an enzyme called DNA polymerase.
We use the E gene primers in both steps so that only RNA from the virus is copied, and nothing else.
This video shows you how RT-PCR works.
How do we find out if the virus RNA has been successfully copied?
The testing laboratories do 45 "cycles" of PCR on a Covid-19 test sample, which takes a little over half an hour. After this time, a single SARS-CoV-2 RNA molecule will have become 17 million million identical DNA molecules. These are so small that you STILL can't see them with your eyes.
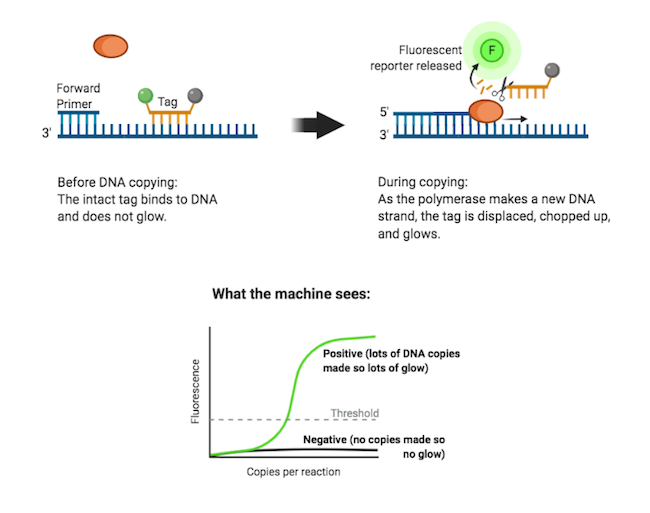
To see how much DNA there is, and to find out if the test is positive, the PCR reaction mix includes a special tag that glows when it is cut up.
The tag sticks to the same piece of DNA as one of the primers.
When the DNA gets copied, the tag is knocked off the DNA and gets chopped up. The unstuck, chopped-up tag then starts to fluoresce (glow).
These tags can be 'seen' and measured by a machine that detects light. The more fluorescence detected from a PCR reaction, the more DNA copies have been made.
So when there is a lot of glowing, you know that coronavirus RNA was in the swab sample and lots of DNA copies were made, and therefore that the test is positive.
If there is no glowing, there wasn't any coronavirus in the swab sample, no copies of DNA could be made, and the test is negative.
Do many tests all at the same time (Get in the robots!!!)
A really important part of testing for coronavirus is that we can carry out many tests as quickly as possible.
Our testing laboratories do this by getting robots to do the RNA preparation and the reverse transcription PCR.
One person can process maybe 100 samples by hand each day, but a robotic machine, once it has been set up correctly, can carry out as many as 1000 tests in 24 hours, and is not as likely to make mistakes.
This is one of the robot testing machines that we use in New Zealand:
Questions about PCR tests for the new coronavirus
What happens if we run out of test kits from overseas?
Our friends next door in the Otago Department of Microbiology and Immunology have helped to get this test up and running in New Zealand. They have designed it to work with enzymes and other reagents that we can import from overseas.
But what happens if there are shortages of some of those reagents from overseas, and we can't import them for a while?
Health workers, scientists and the media have highlighted this as a problem that we need to think about. (Read the article on RNZ: Covid-19: Limited testing kits has scientists searching for generic alternative.)
We can make important parts of the test here in New Zealand if we needed to.
This is where the skills and equipment in research institutions like Otago Biochemistry can help out.

Sam Jamieson purifies reverse transcriptase enzyme in the Mace lab.
In Otago Biochemistry we have already been practicing making enzymes just in case. Associate Professor Peter Mace's research group has already made the reverse transcriptase enzyme.
They put the gene encoding the enzyme into some bacteria, got the bacteria to make the enzyme, and then extracted the enzyme out of the bacteria.
Scientists often make proteins in this way so that we can study them and find out how they work.
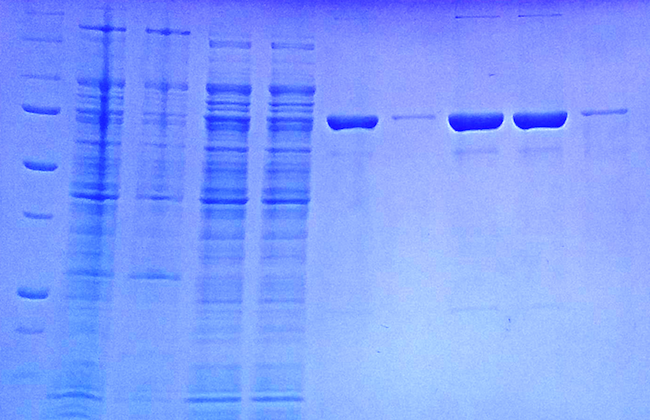
A photo of a gel that shows the enzyme at different stages during purification. The big blobs on the right are samples of pure reverse transcriptase enzyme.
Can the PCR test distinguish between Covid-19 variants?
While it would be possible to design a PCR test that would distinguish between several known Covid variants, the ones we use do not.
To find out which variant has produced the positive test, a complete genome sequence is determined. PCR makes lots of copies of one small piece of DNA, but genome sequencing “reads” the entire 30,000 base (bases are often called “letters” as they are written as A, U, C & G) sequence of the viral RNA using a different process. This is how new variants are discovered, and how we trace connections between cases. When the virus replicates in our cells it sometimes makes mistakes. This is how it evolves - and indeed how humans, plants and every other living thing evolves.
Most mistakes make little or no difference to the way the virus acts, but we can see them when we sequence a sample. If two samples from different people have exactly the same sequence, we know that the people are very closely connected - it's likely that one of them caught the virus from the other. If there is only one base difference between two samples, we know they are very closely connected too. If there are five differences then there will be many steps of infection between the two people.
Some mistakes do make a difference, and if that difference is an advantage to the virus then that ”variant” becomes dominant. Usually this will not be a single base mistake, but more often a combination of several that have accumulated over a period of time. This has happened with the Delta variant. We are watching evolution happen.
There is more information on Covid genome sequencing in New Zealand here: https://www.esr.cri.nz/our-expertise/covid-19-response/new-news-page/
Who controls the PCR test in New Zealand and all data that comes from it?
The testing is done in all sorts of testing laboratories, in hospitals and at the Institute of Environmental Science and Research (ESR) NZ. Every laboratory that performs tests needs to be accredited by International Accreditation NZ (IANZ). All test results go into the NHI database that holds everyone's medical data and is available to the medical profession. Your GP might belong to an online portal that allows you to access your own test results.
What is the exact 'amplification rate' for Covid-19? What is the CT number they use in NZ?
There are in fact hundreds of different commercial PCR test kits available around the world, and not all of them work the same way. This answer is applicable to most of them, and to all the tests performed in New Zealand.
There is a lot of mis- and dis-information floating around the internet regarding CT values. The robots that perform the PCR tests do run for 40 cycles, but results are NOT given as positive or negative at that point.
The number of cycles run is irrelevant. Hundreds of reactions are run at the same time and the PCR reaction is monitored in real time.
Results are given as a CT (cycle threshold) number, which is the number of cycles it took for a positive result to appear.
A low CT number = lots of virus
A high CT number = very little or no virus
If a sample gave a positive result within less than 25 cycles, it would be regarded as “positive”. If the positive result appeared after 25 cycles and before 35 cycles, it would be regarded as suspicious and the person tested again.
The higher the CT number is, the less of the original viral RNA was present, and a high CT number can mean one of two things - either the case is historical and the test has picked up viral fragments that are no longer infectious OR it is a very new infection and the viral load is still low. A second test from a new sample will show which of these is the case - in a new infection the second test will give a much lower CT number, which shows there is more virus in the sample.
You will have heard Dr Bloomfield talking about “historical cases” and “weak positives” - this is what he is talking about.
In NZ we have few enough cases of Covid that we are able to do all these follow up tests, and also to sequence the genomes of all our positive cases. In other countries this is not necessarily true.
Below is an annotated image of real time PCR results - in this case they are not testing for Covid, but for the amount of beef in processed meat - however the principle is the same.
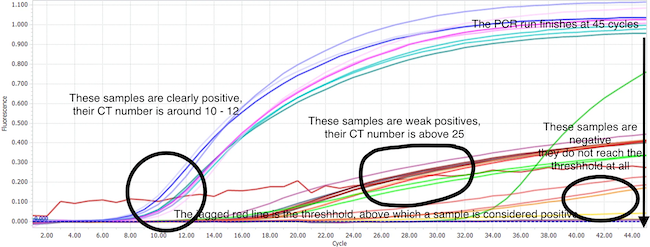
Should CT test results with a CT value over 35 be ignored?
If you look at the covid PCR test evaluations (none of which are ones used in NZ) at https://www.finddx.org/covid-19/sarscov2-eval-molecular/molecular-eval-results/ you will see that the CT numbers for 1-10 molecules of RNA vary between 30 and 40.
So to say that anything over 35 shouldn't be looked at is not necessarily correct.
You must remember that people whose tests have high CT numbers are re-tested, and only classed as positives if the CT value is lower on the second test.
It is also possible to have a false negative test, and if the person shows all the signs of having covid and has been somewhere they could have caught it, they will be retested even if their PCR test returned a completely negative result. False negatives can happen when the original swab didn't pick up any virus, this can happen if the infection is based deep in the lungs instead of in the nose, or even if the patient flinched while being swabbed! False negative results are much more common than false positives.
There is an article here that answers some questions about CT numbers and “weak positives”: https://www.stuff.co.nz/national/health/coronavirus/122865913/when-is-a-covid19-test-result-a-weak-positive- why-more-of-them-are-being-found-and-how-the-cases-are-dealt-with
Dr Bloomfield gives the numbers: under 25 for a positive, around 30 for a query, and over 35 for a historic case. But again, if the person does not give a positive test result but has been exposed to Covid-19 and is displaying symptoms, they will be retested no matter how high the CT value of the original test was.
Where is the data displayed? How do pooled tests work?
The data on individual tests is not displayed anywhere in public. Most tests are not even “individual”.
To enable laboratories to process huge numbers of Covid-19 tests they frequently pool samples. They extract samples from people individually, they then take a small portion of each sample combine them with several other samples together in one tube. Then they do the PCR reaction on the pooled sample. Remember - they have only used a small fraction of the initial sample for this, they may need to use the rest later on.
While we have very little Covid-19 in the community in New Zealand nearly all of the pooled tests will give a negative result, and because the test is sensitive enough to detect one positive sample in a pooled sample, a negative pooled sample means all of the individual samples are negative.
If a pooled sample gives a positive result, the samples that made up the pool are then re-tested individually to find the positive one(s).
It's really very clever and saves a lot of time and money (these tests are really expensive to do, if you need one for travel it'll cost you over $200).
Of course, if they have reason to believe that a sample WILL be positive - e.g. people with symptoms who have been at “places of interest” it's faster and more efficient to test them individually to start with, so that's what they do.
There is more information on Covid testing at the Ministry of Health: https://www.health.govt.nz/our-work/diseases-and-conditions/covid-19-novel-coronavirus/covid-19-health-advice-public/assessment-and-testing-covid-19/how-covid-19-testing-works
Can a positive test tell us if the person is currently infectious or how ill the person is likely to become?
Viruses aren't actually living things, very simply put, they're bundles of self replicating genetic material wrapped up in protein. They can't make their own proteins, they have to hijack a living cell's “machinery” to do that.
When the body mounts a successful defence against the virus, virus particles break down, releasing the genetic material and proteins into the body. This debris is then cleared away by normal cellular processes, but some of it can become trapped in nooks and crannies of the nose and throat.
When laboratories test for the presence of the virus they are actually detecting the presence of genetic material (RNA), and part of the preparation for that is to break up and wash away the proteins and membranes surrounding it.
So you can see that it would be impossible to tell whether or not the RNA that has been detected was originally in an intact viral particle (infectious) or just floating around by itself (not infectious) in the mucus being tested!
Because most viral debris is cleared away by the body quite quickly, we can say that if there is lots and lots of RNA present - a low CT number - it is almost certain that that RNA came from viruses that are currently part of an infection.
As for how ill the person is likely to become - that is a function of the person, and of how many virus particles they were first exposed to. Everyone is different, every body's reaction to infection is different, and there is just no way to predict what it will be. Just as some people get very sick with mumps while others don't know they've even had it.
Is it true that the CDC in the USA have banned the PCR test because it can't tell the difference between Covid-19 and the flu?
No.
The CDC have advised that they will not be applying to have the emergency use authorisation for the PCR Covid-19 test they provide extended beyond December 2021. This is because they are replacing it with a combined PCR test that can detect both Covid-19 and two strains of the flu.
The PCR test the CDC provides is just one of hundreds, and they recommend that labs who use their standard test at present should replace it with a combined test - either theirs or one from another provider. The combined test gives more data about respiratory diseases - the CDC like to know how much flu is around as well as how much Covid-19.
The table below sets out what the different tests will show:
| Standard Covid-19 PCR test result | Combined Covid-19/Flu PCR test result | |
|---|---|---|
| If you have Covid-19 | Positive | Positive for Covid-19 |
| If you have Influenza A | Negative | Positive for Influenza A |
| If you have Covid-19 and Influenza A | Positive | Positive for Influenza A and Covid-19 |
| If you have Influenza B | Negative | Positive for Influenza B |
| If you have Covid-19 and Influenza B | Positive | Positive for Influenza B and Covid-19 |
| If you have Influenza A and Influenza B | Negative | Positive for Influenza A and Influenza B |
| If you have Influenza A and Influenza B and Covid-19 (highly unlikely!) | Positive | Positive for Influenza A and Influenza B and covid-19 |
| If you have a cold or some other disease, but not Covid-19 or the flu | Negative | Negative |
Here is the CDC's announcement.
Here is information about the new combined (multiplex) test they are providing.
There is an amazing amount of research being carried out on the new coronavirus around the world. We have put together a collection of links to useful websites that explain what the virus looks like, how it works, how to test for it, what treatments and vaccines are being developed, and more on our Useful information about the new coronavirus page.
You can read and watch more stories about research at Otago Biochemistry on our School Resources page.
Contact us with any suggestions to improve or add to this page at biochemistry@otago.ac.nz.
